One Step at a Time
Why could my 14-year-old suddenly not walk?
As told to Faigy Peritzman by Anna King
You never know what’s going to happen from one day to the next. Looking back to the winter of 2013, it’s clear my life has been divided between “before” and “after.”
Our family of seven (five daughters) had just moved to our new apartment on a yishuv outside of Yerushalayim. The morning after Chanukah vacation, my 14-year-old daughter, Ariella, woke up not feeling well. I was running around trying to get everyone out on time despite the back-to-school sluggishness and didn’t pay much attention to Ariella’s complaint. She didn’t seem that sick and I figured maybe she just needed another mental health day before going back to school.
Yet on day two, Ariella still hadn’t come down from her second-floor bedroom, claiming she felt too weak. And on day three I knew we needed a doctor and quickly. I made an appointment with our GP at the yishuv clinic. At this point Ariella literally could not stand up. We carried her to the car, but when we got out at the clinic, she fell to the ground, scraping her ankle very badly and bleeding heavily.
The staff tended to her ankle and then we had our appointment with our doctor. He had no clue what was going on, but decided he’d send her for blood work. There happened to be a visiting orthopedist at the clinic at that time so we consulted with him as well. He also was stymied, but didn’t think this was an orthopedic issue and thought we should head straight to the ER. We thought he was overacting, and decided to come back in the morning for the blood work and then make a decision based on that. But while the blood work showed nothing out of the ordinary, we had reached day five and it was clear something was very wrong.
We traveled to the hospital and were admitted to the ER. Ariella had to sit in a wheelchair; although she was able to shuffle her feet a bit to move a few feet, there was no way she could traverse the hospital corridors. My husband is a Kohein and avoids hospitals whenever possible, so it was me hauling her into the wheelchair — and she is taller than I am.
The ER staff took one look at her and began bombarding her with questions. Had she eaten anything different recently? Had she taken a vaccine recently? At one point they even sent me out of the room to ask her more personal things that perhaps she didn’t feel comfortable admitting with me around. They were afraid she was on drugs and wouldn’t admit it.
Finally, when the battery of tests and questions all showed nothing out of the ordinary, they admitted her to the pediatric ward and basically decided to wait and see what would happen next. What happened next was that things got worse.
Up until now the weakness Ariella was experiencing was mostly in her arms and legs. She couldn’t lift her arms to feed herself or brush her hair or take care of herself and her legs weren’t strong enough to hold her up. I was doing everything for her, lifting her, feeding her, helping her to the bathroom. It seemed we had hit rock bottom. But after a week of this, we realized rock bottom would get lower. Half of Ariella’s face became paralyzed.
I was petrified. The doctors were murmuring about the possibility of multiple sclerosis, but her symptoms didn’t really add up. Finally the doctors announced the diagnosis: Guillain-Barre Syndrome GBS (see sidebar).
That did seem to make sense. A GBS attack can happen suddenly, and symptoms can range from the inability to move one’s limbs, like Ariella, to paralysis affecting the pulmonary muscles, which can lead to intubation. The hospital did check Ariella’s breathing ability, and although it was a bit below normal, baruch Hashem it was sufficient.
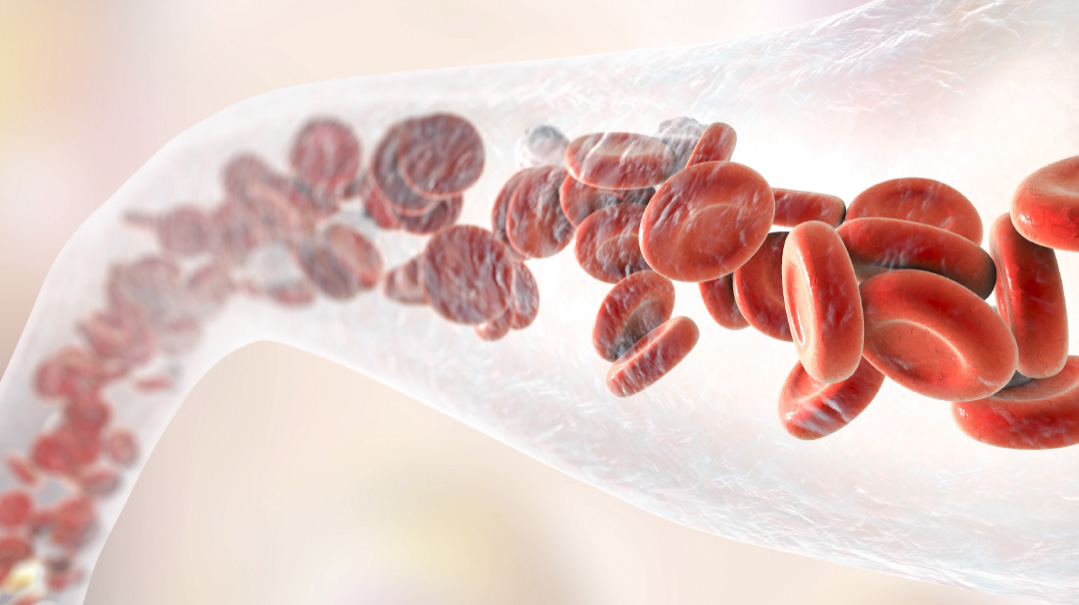
The doctors proceeded to treat her for GBS, giving her IVIG treatments (an infusion of donated blood that contains healthy antibodies) intravenously. But it didn’t seem to make any difference. They also gave her a low dosage of steroids, also recommended treatment for GBS, but that, too, didn’t seem to fix the problem.
At this point we had been in the hospital for four weeks. Any sense of normal life had ground to a standstill. I work as a doula but had to cancel all my appointments, as I was spending all my time with Ariella in the hospital. My husband was trying to work and keep the rest of our family running. Our kehillah, rav, and neighbors rallied to help our family, but we were still at a loss.
As time passed, we began doubting the GBS diagnosis. While a GBS attack may be terribly debilitating, after the initial attack the patient begins to show improvement as the symptoms fade. However, in Ariella’s case, the symptoms were growing worse, not better. Still, the hospital stuck with its initial diagnosis. They decided to discharge us and send us to a pediatric rehab facility. We traveled by ambulance, not realizing this was going to be our home away from home for a long time.
Ariella’s schedule in rehab was daunting. She had therapy sessions from nine a.m. until four p.m. in all different areas: hydro, physical, occupational, emotional. The facility also scheduled family therapy and it was a lifesaver; we were reeling from the many changes the past month had wrought. Ariella was given a beautiful room with huge windows. As the weather warmed, we’d sit on the balcony of our room against a picturesque background of tall green pine trees and wispy white clouds. I felt that we had arrived at a good place and were ready to heal.
Ariella’s roommate was an Arab whose mother spoke no English or Hebrew. Yet our mutual circumstances forged a bond that surpassed politics. At one point I was at a low, feeling so despondent with our situation that I was breaking down. The Arab woman patted me on the back and pointed upward, a completely nonverbal communication, reminding me of where my help was really waiting.
Despite the many hours of therapy, Ariella still wasn’t making that much progress. At one point we were given an appointment with a famous pediatric neurologist who had a clinic in the hospital. He was a very experienced doctor, who was always surrounded by medical students as he pontificated on the various patients’ conditions.
We were called to his room where there were approximately ten medical students observing the consultation. The doctor told Ariella to stand up. She responded that she couldn’t. “Of course you can!” he said and proceeded to haul her up from her wheelchair. She immediately collapsed onto the floor. Nonplussed he turned to the students. “Classic GBS,” he declared. I was horrified.
That painful incident highlighted what we were realizing; no one was concerned with the discrepancies between the diagnosis of GBS and the progress Ariella wasn’t making.
Almost no one that is. Yamima, Ariella’s physical therapist, was originally from England and took a great interest in Ariella’s progress. It was she who questioned the GBS diagnosis and kept asking if we’d reconsidered the original diagnosis. In clear Hashgachah, she was also working with a different patient who had been admitted to the facility a short while before Ariella. This child had been diagnosed with CIDP (Chronic Inflammatory Demyelinating Polyneuropathy; see sidebar). Comparing the similarities between the two cases, Yamima persistently suggested to us that we pursue this diagnosis.
Things were coming to a head and although we agreed with Yamima’s points, still it seemed every major doctor out there was convinced Ariella had GBS. Yamima suggested we consult with another doctor, Professor Nevo, who worked in Hadassah Mt. Scopus.
We consulted with our rav and with a very big bikur cholim organization, and they were both concerned that Professor Nevo would not have time to review our case. The rav and the askan both suggested we see someone a bit lower down the totem pole who would take a more personal interest in our case. What we didn’t know was that Professor Nevo was the leading international pediatric expert on CIDP.
Despite Yamima’s insistence, we went ahead and booked an appointment with a different neurologist in Hadassah Mt. Scopus. Imagine our surprise when we arrived on the day of the appointment to find the doctor we expected, and Professor Nevo, both waiting for us in the room. The doctor said he’d asked Professor Nevo to sit in on the consult because it was clear that our case was complicated. And sure enough, about halfway through the intake, this doctor said he was bowing out, that this was way beyond his field, and he insisted Professor Nevo take over. Just like that, Ariella became the professor’s patient.
Sure enough, as he listened to our story, he was convinced that GBS was an incorrect diagnosis and that the accurate diagnosis was CIDP. CIDP is much rarer than GBS, and Ariella had to undergo many painful neurological tests to confirm this diagnosis. The testing took place over the course of two weeks and included such painful procedures as a nerve conduction test, which tested Ariella’s nerve endings with electric shocks to see how they’d respond; it was as horrific as it sounds. Since Ariella was so young, and these tests were so painful, most were done under some sort of anesthesia, which necessitated hospital stays and more pain.
To everyone’s surprise (except Professor Nevo’s), Ariella tested positive for CIDP. In addition to it being a rare condition, CIDP rarely affects a young teen like Ariella. But despite the odds, Ariella clearly had the condition.
Knowing the proper diagnosis and having the world’s pediatric expert on this condition on our team was a game changer. Professor Nevo prescribed higher than normally prescribed levels of steroids, which helped her recover. In the first few days of the steroids her face paralysis began to lift.
Yet the steroids came with serious side effects, with Ariella suffering from bloating and contending with mood swings. He also prescribed higher dosages of IVIG medication to prevent further attacks. The medication was given once a month in the hospital, intravenously, taking about 14 hours each time. The cost was exorbitant: 60,000 shekels per infusion. And at first our insurance refused the treatment. I went to battle, working my way higher and higher through insurance administration, until I reached the head offices in Tel Aviv. I insisted they give her the treatment, pointing out that if chas v’shalom Ariella had another attack, they’d be paying much more in the long run for her treatment and physical therapy. B’chasdei Hashem, they finally approved the treatment.
At that point, we were staying in the rehab facility throughout the week and coming home for Shabbos. My husband would carry Ariella up the stairs to our house, and she’d sleep on the main floor sofa over Shabbos, before heading back to rehab Sunday morning. I was spending all day with Ariella, but at night I had to go back to my other children. Yet Ariella literally couldn’t do anything for herself. One of the girls in her older sister’s class arranged a rotation of 11th and 12th graders who would each spend the night with Ariella, caring for her until I could come in the mornings. It was incredible what a difference this chesed made for us.
We had been in rehab for four months when Ariella was finally discharged to outpatient therapy, three times a week. The steroids were helping, and over that summer she was able to do more and more. Still, it took months to wean her off the steroids, a difficult process itself. Finally, at the end of that summer, Ariella was able to walk and even to climb stairs, albeit very slowly and with poor balance. She also attended Camp Simcha, enjoying herself for the first time in months.
Ariella had missed most of ninth grade, and now we had to make plans for the future. It was clear she would not be able to return to her high school in Yerushalayim, and we made arrangements to switch her to the local school on our yishuv. The municipality came through for us, first sending tutors to our house for homeschooling, and then later modifying the school building so Ariella would be able to attend, and providing her with bus service to and from school. It was wonderful that Ariella was able to return to a normal schedule but painful to know that all her hard work was in jeopardy, as she was susceptible to an attack at any time.
She managed to make it through a whole year before the next attack came. By now Professor Nevo was heading the neurology department in the famous Schneider Children’s hospital in Petach Tivkah, and so he had her hospitalized there under his auspices. He didn’t want to put her back on steroids and after it was clear that IVIG wasn’t working as effectively anymore, he instead prescribed a procedure called plasmapheresis. To describe this in layman’s terms, it’s basically like a blood rinse. Ariella would lie on a bed, with her blood and its treacherous attacking antibodies being emptied from her body via one arm, and in her other arm she would receive transfusions of healthy antibodies and new plasma. Thankfully, the procedure was helpful and we were discharged from the hospital, though she had to do it again every two months for a year, after which she was able to stop.
Ariella is still susceptible to attacks at any time, without any warning. We see Professor Nevo every three to six months. He’s developed a good kesher with Ariella, and the entire staff of Schneider greets her and cheers on her progress whenever she visits the hospital.
We try to pay back the kindness as well. At one point Professor Nevo asked us if he could feature Ariella at a convention of neurologists from all over the country. They meet every few months and highlight interesting cases to learn from them. Despite her natural reluctance, Ariella agreed to be showcased and walked onstage before all these professors to show them what progress could be made. Despite the rareness of CIDP, studies show that it is more prevalent for some reason in Israel, across all demographics, and if we could help someone else with this condition in some way, we wanted to be part of it.
It’s been a long haul since those tumultuous years. B’chasdei Hashem, Ariella is now in her twenties and has not suffered another attack. Yet she is disabled, with limited mobility and balance, often falling and suffering from those wrenching spills.
Still, she’s determined to live independently, sharing an apartment in Jerusalem where she works. Her job is accessible and attuned to her needs and it’s a huge comfort knowing she’s happy where she is and with what she’s doing. Yet she’ll always be at risk for another sudden, surprise attack.
We try not to let our worry get the better of us, and aim to focus on what is going on at the moment, appreciating every day and not worrying about the future. As a doula, I often tell my clients that while the pain of contractions can be hard, the payback is so worth it. Similarly, Ariella and our family know that the pain and difficulties that come with living with a disability are huge and often distressing. Still, we focus on the moment and the appreciation and enjoyment of each day at a time.
Please daven for Ariella Hadassa bas Leah Chasha for a refuah shleimah.
What is CIDP?
Chronic inflammatory demyelinating polyneuropathy (CIDP) is a rare type of autoimmune disorder in which the body attacks its own myelin sheaths — the fatty coverings on the fibers that insulate and protect nerves.
CIDP is similar to the more commonly known disease Guillain-Barre syndrome (GBS), which also attacks the myelin sheaths. However, GBS is generally considered a short-term disease, where the body recuperates after an attack, while CIDP is considered a chronic, or long-term, disease.
CIDP is usually divided with these three classifications:
Progressive, where the disease continues to worsen over time
Recurrent, where there are episodes of symptoms that stop and start
Monophasic, where there is one attack of the disease that lasts one to three years, but doesn’t recur
What causes CIDP?
It’s unclear what causes CIDP and there doesn’t seem to be a genetic link. Although it can occur in anyone, the disease more commonly targets those in in their 50s and 60s, while men are twice as likely to have it than women.
Signs and Symptoms:
Tingling and weakness in the arms and legs
Loss of reflexes and balance, affecting walking
Numbness in legs and arms
Because CIDP is similar to GBS, the confusion can delay a proper diagnosis.
Diagnosis:
To confirm CIDP, the following tests are usually run:
Blood and urine tests
Nerve conduction study, also called an electromyogram. This uses low electrical currents to test nerve function and response.
Lumbar puncture. Cerebrospinal fluid (CSF) is withdrawn from the fluid around the spinal cord, testing for elevation of certain related proteins.
Treatment
Treatments for CIDP include: immunosuppressive drugs, steroids, intravenous immunoglobulin, and plasma exchange (plasmapheresis) to remove immune system proteins from the blood.
Without treatment, one in three people with CIDP will become wheelchair-bound. Therefore physical and occupational therapy are also essential.
Information courtesy of Johns Hopkins Medicine
Did you ever have a medical problem that you were told “is nothing to worry about,” and it ended up being a serious issue? Did you have symptoms that stymied doctors? We believe sharing our journeys can bring awareness, empathy, and a sense of connection to those who’ve gone through a medical crisis. If you had a medical mystery and would like to be part of this column, please send a brief description of your story to familyfirst@mishpacha.com
(Originally featured in Family First, Issue 832)
Oops! We could not locate your form.