Immune to Despair
I had no symptoms, but a blood test sounded the alarm
As told to Faigy Peritzman
I’m an action person, a shaker, a mover. I pay attention to details, pull strings together to tie them in neat bows, and when I do encounter problems, I push myself to solve them.
So it was both humbling and life-altering to be diagnosed with a chronic life-threatening condition at age 21, one that all the willpower in the world couldn’t wish away.
Together with this stark realization came a loss of hope. Yet once I reached rock bottom, once I was able to let go of that gossamer line of shiny hope, I was able to move on to acceptance. And that’s when my real journey in growth started.
My story started out innocuously enough. I was the average teen, busy with friends, family, school — just regular everyday life. Then in tenth grade, during a routine blood test during a checkup, I discovered that I was suffering from ITP.
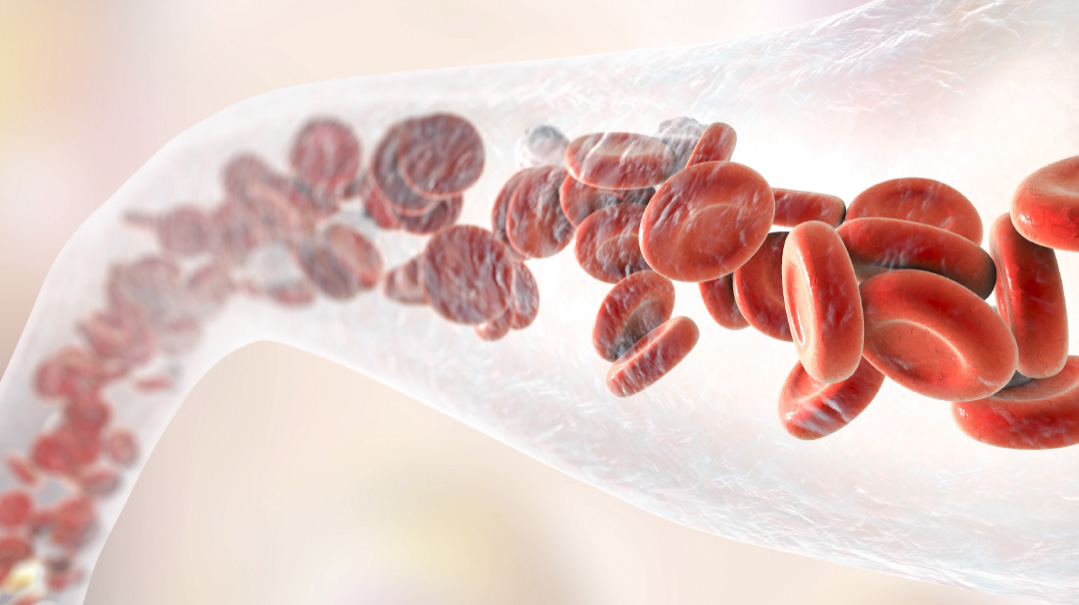
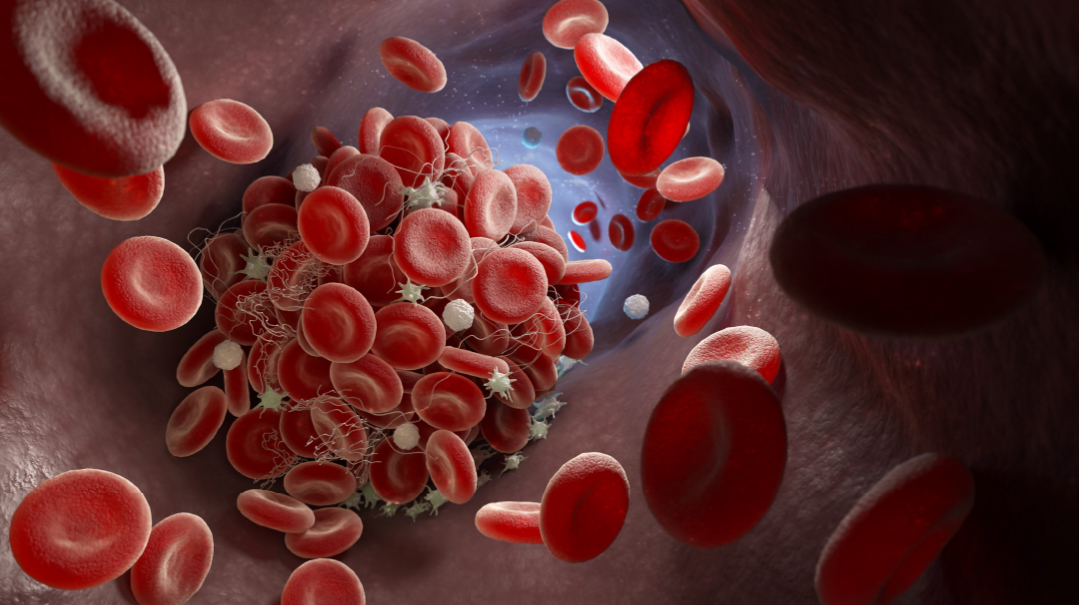
ITP (immune thrombocytopenic purpura) is a blood disorder in which a person’s platelet counts are very low. A person needs platelets to help the blood clot and stop bleeding. A person with a low number of platelets can bruise easily, and simple cuts or abrasions can be very dangerous. Critically low platelet counts put a person in danger of hemorrhaging, even internally.
Still, many people have low platelet counts, and there are treatments to take care of this issue. I was prescribed a monthlong regimen consisting of four weekly infusions of rituximab plus dexamethasone, and every second week, additional doses of daily oral dexamethasone. Afterward, I was instructed to follow up on my platelet count by doing bloodwork every six months, which I did.
My hematologist, Dr. James Bussel, was a great guy. He reassured me that the ITP was under control and that other than those biyearly blood tests, I was good to go. But soon after I got my diagnosis, Dr. Bussel retired, and I didn’t bond well with the new hematologist. On several occasions, my platelets level dropped, but she didn’t seem overly concerned. “If it goes under the 30-count, we’ll treat it,” she’d say dismissively. (Normal platelet results are between 150,000 and 450,000.) Since my numbers never dropped that low, I took my doctor’s advice and just ignored things.
When I came back from seminary, I was no longer under the care of that pediatric hematologist, as I’d turned 18. Instead, I went to see a new adult hematologist in a clinic at the same hospital.
I didn’t anticipate any major news from that first appointment. Everything had been great in seminary; I had no new symptoms, and I was ready to meet this new doctor, do my bloodwork, and go home for the next half a year.
But a few minutes after drawing blood I was immediately called into the doctor’s office.
“Your platelet levels are dangerously low — they’re at three,” the doctor said starkly. “You’re in immediate danger of hemorrhaging at any point, and unless you go directly on dexamethasone right now, here in my office, I will have to admit you to the hospital immediately!”
I was shocked. I showed none of the classic signs of such a low platelet count, no bruising or bleeding gums, etc. And I definitely did not want to go back on dexamethasone. When I had been on it in tenth grade it had wreaked havoc on my moods and emotions, and I was not prepared to start that again.
But the doctor was adamant. She would not let me step out of her office without either agreeing to a full dose of intravenous rituximab and dexamethasone right then and there, or I would end up in the hospital. With no choice, I gave in and was hooked up to the IV. It felt like poison surging through my body. I was really shaken up.
The doctor also ordered more extensive bloodwork than I had been doing before. All along I’d tested my platelet count biannually. But now, a more comprehensive scan of my bloodwork revealed that my body wasn’t producing antibodies properly. Even the antibodies from common children’s vaccinations that I had taken as a kid were not showing up in my blood.
Concerned, the doctor suggested I revaccinate against these diseases. Since Covid was raging, too, I also received three vaccinations against Covid. Yet when my blood was analyzed, even after being revaccinated with shots such as MMR and DTP, none of these antibodies showed up in my system.
That’s when I received the verdict that would change my life. I was diagnosed with primary immunodeficiency (PI; see sidebar), which meant that my immune system was not working correctly. My body could not produce its own antibodies, and as such, it was completely physically incapable of protecting itself against any sickness. Even something as mild as a cold or a virus could kill me, since my body could not fight back.
It was impossible to know when, exactly, this had started. It’s possible it had all started back in tenth grade when I had been receiving rituximab. The purpose of that drug is to wipe out the T-cells in the body to encourage platelet levels to rise. In most patients, the body then reproduces those T-cells. In my case, my body simply did not. Since T-cells are responsible for the body’s immune system response to threats, I was now at a real risk without T-cells.
At the time, even listening to the doctor explain these harsh facts, there was a part of me that was completely in denial. Hey, I rationalized, I’d never even gotten Covid and everyone I knew had gotten it already. Obviously, my body was perfectly healthy.
My doctor wasn’t having any of it. “You are walking around like a ticking time bomb,” she said sternly. “It’s like driving without a seat belt. Sure, you may get out of the car safely 99 percent of the time, but that one percent would be all it takes to kill you.”
What were my options? What did one do without antibodies? She explained to me there was a treatment called IVIG. Basically, I would receive the plasma of healthy blood donors by intravenous drip and that would provide my body with the antibodies I needed. Since I was not producing any antibodies, I would need to undergo IVIG every four weeks.
“For how long?” I asked the doctor innocently.
“For as long as you want to live,” she said.
Still not completely convinced, I started researching. I also went for a second opinion. My old hematologist, Dr. Bussel, had since retired, but his wife, Dr. Charlotte Cunningham-Rundles, is a top immunologist. She agreed with the diagnosis of PI and the treatment plan of IVIG.
Still, even with the facts laid out so starkly in front of me, I couldn’t yet accept them. I was still hanging on to hope that this was all a mistake, a glitch, and that at some point my body was going to kickstart itself and begin making antibodies again.
I was young, I had things to do, places to go, my whole future ahead of me. I didn’t have time, patience, or even the maturity to stand there and say, Hey, you’re sick with a possibly fatal illness — take care of yourself. I simply couldn’t swallow that.
So for the time being I did nothing. I felt fine! Great! Why was everyone making a big deal out of something that would go away by itself?
My parents didn’t know what to do. They realized the gravity of the situation, but they also knew we couldn’t proceed further until I would realize the necessity of protecting myself.
IVIG is a painful procedure that takes several hours. I needed to agree, to be ready both mentally and physically to start the treatments, and then to keep on going with life in spite of them. But at that raw moment, I was simply in denial.
My family rallied, and my friends spoke with me, some calmly, some more emotionally, until finally, that armor of denial began slowly to crack. I had an incredible friend and mentor who helped me immensely during this process and gave me a strong hand to hold. Slowly, I began to realize that all these people really cared about me. And they were all adamant that this is what I needed to do to… well, yes, I finally could say this… I needed to do this to stay alive.
With that loss of hope came acceptance. I had a chronic condition that could be fatal if I didn’t take care of it. Yet with that admission came a greater acceptance, of myself, my place in life, and my tafkid in the grand scheme of Hashem’s world.
I was not going to let my diagnosis define me. Neither was I going to let it kill me. Yet what it did do to me is make me realize how intricate and complicated each person’s journey in This World is. I’d never have imagined I would be a person showing up at the hospital once a month. The treatment is brutal, the nausea is incredible, and when I’d finally get home from the hospital, I’d be weak and sick for about three days. And this goes on every single month.
But I was determined. I had a great job I loved, and my bosses were amazing at allowing me to work when it was best for me. I put in many long hours on weekends and late-night sessions, times when my creativity peaks and I’m on a roll, working and accomplishing and on a professional high. Then come those three days a month where I lay low, keep work at a minimum, and remind myself that this too will pass.
It’s a strange sort of existence. And no one understands just how brutal daily living is, how much strength I need to push myself. Sometimes I feel so sick and simply can’t function.
Since I am receiving blood from a bank of donors, sometimes the actual blood I receive can also make me sick because my immune system is so weak.
The physical hardships aside, though, I find the most challenging part of my journey is that it’s so lonely and painful. I actually don’t know anyone my age who has PI. Most patients are much older; undergoing IVIG so regularly at my age is very rare. Many insurances won’t even approve the treatment unless it’s clearly lifesaving, as it is in my case. So no one really understands how these hours-long treatments rip me to pieces. When I’m done, I get up, drive home, and put a smile on my face, because this cheerful mask is essential. But I feel so isolated.
The understanding I’ve gained has spurred me to reach out and give support to others who are going through their own journeys. And that’s the main reason I’m sharing my story: it’s with the hope that perhaps I can help support or share pertinent information with someone else. I want to alleviate the pain and suffering that go hand in hand with any medical saga. If I can help even one person, this journey becomes all that more rewarding.
This is my life, and yes, I’ve fully accepted it. I know I’m growing in ways that my “normal” contemporaries aren’t. I know life is full of ups and downs and journeys that we never planned on taking. But I also know that once we’ve accepted these journeys, they can lead us to vistas and destinations we never dreamed of.
What Is PI?
Primary immunodeficiency is a condition characterized by a weakened immune system, allowing infections and other health problems to occur more easily.
Some people with primary immunodeficiency are born missing some of the body’s immune defenses or with the immune system not working properly, which leaves them more susceptible to germs that can cause infections. Others do not have a genetic component.
So far, researchers have identified more than 300 forms of primary immunodeficiency disorders. Some forms are so mild they can go unnoticed until adulthood. Other types are severe enough that they’re discovered soon after a person is born.
These types can be divided into six groups based on the part of the immune system that’s affected. It’s possible to be affected by more than one.
B-cell (antibody) deficiencies
T-cell deficiencies
Combination B- and T-cell deficiencies
Defective phagocytes
Complement deficiencies
Unknown (idiopathic)
Signs and Symptoms
Signs and symptoms of PI differ depending on the type of the disorder, and they vary from person to person.
One of the most common signs of PI is having infections that are more frequent, longer lasting, or harder to treat than those of someone with a typical immune system. (A person may also get opportunist infections, which are infections that healthy immune systems aren’t susceptible to at all.)
These infections can include:
Frequent and recurrent pneumonia, bronchitis, sinus infections, ear infections, meningitis, or skin infections
Inflammation and infection of internal organs
Blood disorders, such as low platelet count or anemia
Digestive problems, such as cramping, loss of appetite, nausea, and diarrhea
Delayed growth and development
Autoimmune disorders, such as lupus, rheumatoid arthritis, or type 1 diabetes
Treatment for PI varies depending on the factors in each case.
(Information from Mayoclinic.org)
Did you ever have a medical problem that you were told is “nothing to worry about,” and it ended up being a serious issue? Did you have symptoms that stymied doctors? We believe sharing our journeys can bring awareness, empathy, and a sense of connection to those who’ve gone through a medical crisis. If you had a medical mystery and would like to be part of this column, please send a brief description of your story to familyfirst@mishpacha.com
(Originally featured in Family First, Issue 876)
Oops! We could not locate your form.