The Hidden Menace
“This child is hypotonic with no gag or cough reflexes. She must go back to the PICU!”

As Told to Faigy Peritzman by Elisheva Braun
If you saw my daughter Leah riding her unicycle with her four older brothers, you’d probably be very impressed with her talent. However, you’d be even more impressed if you knew the hashgachah that occurred ten years ago that led to the healthy, strong Leah of today.
It was a Thursday, two weeks before Shavuos, and six-month-old Leah wasn’t a happy camper. She wanted to be held all day and didn’t want to nurse. Thinking she had an ear infection, I took her to the pediatrician. He checked her, assured me there was nothing wrong, it was probably a virus, and sent us home.
That Friday I could hardly prepare anything, Leah was so cranky. Then my husband and I were up the whole night taking turns holding her and trying to get her to eat. We resorted to giving her drops of milk from a medicine dropper just to get some fluid in her, but even that she’d barely swallow.
By Shabbos morning she was very weak. My husband went to shul and met a neighbor who’s a member of Hatzalah. Upon describing her weakness and dehydration, the neighbor called an ambulance, saying, “You don’t take chances on a baby.”
At the hospital, the nurses couldn’t even find a vein to get blood work or hook Leah up to an IV. Although they kept poking her, she was so lethargic and weak she barely cried.
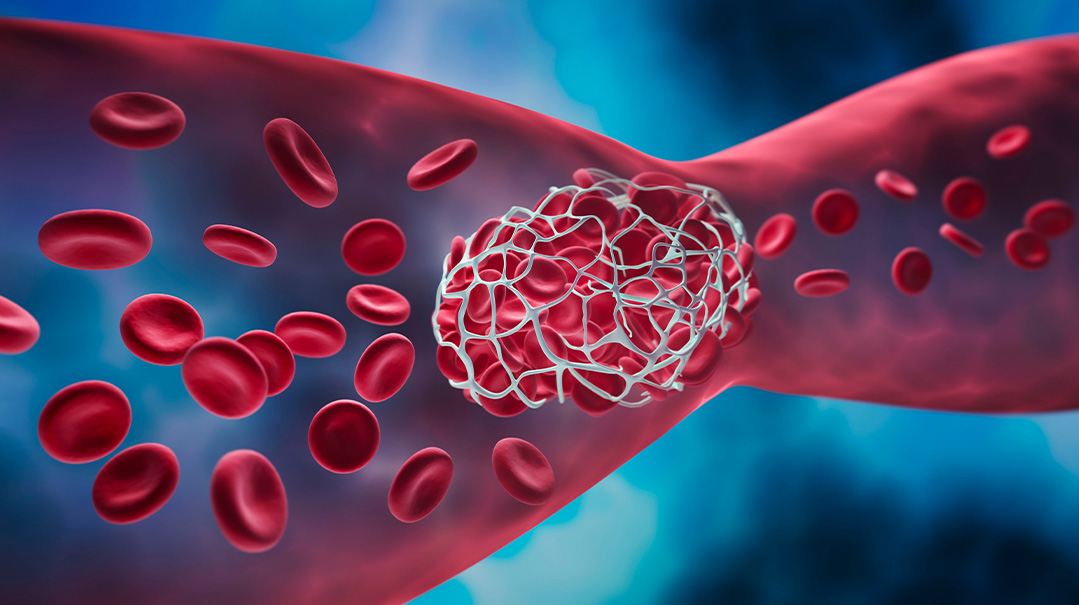
The admissions doctor was perturbed by her inability to swallow and ordered x-rays of her throat. After reviewing the x-rays, a whole group of doctors came to huddle around her crib. Apparently, they were concerned she may have epiglottitis, a potentially fatal condition. If her epiglottis became too swollen or irritated, it could cut off her airways entirely.
They hooked her up to monitors right in front of the nurse’s station to keep an eye on her. Yet, although they were taking all these precautions, it was doubtful she really had this condition, as she didn’t have any of the other symptoms.
After much debate, the doctors decided to do an endoscopy to make a more definitive diagnosis. Such a test would have to be done in the operating room with full anesthesia. It was fraught with risks as well, because if she did indeed have epiglottitis, irritating the condition with a camera would probably stop her breathing and they’d need to intubate her immediately.
It was Shabbos, and we were all alone and so scared. We didn’t know what to do. On one hand, it didn’t sound like this was her condition. On the other, it was clear the doctors didn’t know what else it could be, and shouldn’t we trust the doctors? Reluctantly we agreed to the procedure.
In the middle of the procedure the doctor came out with a smile and said they’d found a gooey white substance in her throat, and removed it. Sure that this was the cause of her inability to swallow, they ruled she didn’t have epiglottis, but thrush.
They moved her to the PICU and decided to treat her with antifungal medications to combat the thrush. The problem was that the medicine was oral, and she couldn’t even swallow her own saliva. They assigned her a private nurse to suction her constantly to keep her from choking.
I still wasn’t comfortable with their diagnosis. A child doesn’t get this sick from thrush. Furthermore, by Motzaei Shabbos, despite the medication, she was getting weaker. She could barely move her head and couldn’t even cry. Yet, every time I mentioned to the doctors that we hadn’t seen any improvement, they brushed me off, saying it takes a baby a long time to get over the effects of full anesthesia.
I was so frustrated. We’d come to the hospital to treat her extreme weakness and inability to swallow, and that hadn’t improved at all; if anything, it was worse! So how was their medication helping? But the doctors were confident they were on the right track and moved her out of the PICU to a regular ward. To combat her inability to eat, they ran a feeding tube through her nose.
Both my husband and I knew something was seriously wrong, but we ran into a brick wall every time we tried to discuss it with the doctors on their twice-daily rounds. They didn’t even come in to see Leah — they just read her chart and made their decisions. I pushed for them to actually see her, to realize how inactive and sick she was, but they huddled in the hallway and kept insisting these were lingering effects from the anesthesia.
They sent me a lactation consultant to help her nurse, but that was a joke; she couldn’t move her head, and certainly couldn’t suck or swallow.
We spent the whole Sunday trying to reach other doctors or organizations to figure out what the real problem was.
That night my husband went back home to sleep so he could get the kids out to school on Monday morning. We were petrified, asking friends and family to say Tehillim, as it was clear Leah wasn’t getting any better. After four boys, I’d waited so long for this little princess, and I was terrified I’d lose her. It was heartening to see how people rose to support us. A friend organized hafrashas challah, another in Eretz Yisrael went to Rav Chaim Kanievsky shlita for a brachah.
My husband’s sister moved our kids into her house so we wouldn’t have to worry about babysitting and food. But that first Monday morning, my husband got the kids off himself. When he took my two-year-old to his playgroup, he mentioned to my son’s morah that his wife was in the hospital with our baby.
“What’s wrong?” she asked, concerned.
Without knowing why, my husband began sharing all the frustrating and scary details of Leah’s condition. As he described her symptoms, the morah said, “Leah must have infant botulism. My niece had it. I’m telling you, no doctor will diagnose her with that condition because it’s so rare, but it sounds exactly like what my niece had!”
As soon as my husband called me with this information, I called the morah’s sister to get more details. She explained that infant botulism is a toxic condition when a baby eats an item contaminated by the botulinum bacteria, and is often found in honey. But I knew Leah had never eaten honey. I’d just started her on applesauce. Could that be the source?
The more this woman shared her daughter’s experience, the more it sounded exactly like what Leah was suffering from. I rushed to the doctor who was making his rounds to share this, but he brushed me off. “No, it’s not infant botulism. In fact, don’t worry, we’ve just ordered an infectious disease specialist to consult on this case, and she’ll tell us her findings this morning.”
The infectious disease specialist expert opinion was that Leah had diphtheria. Diphtheria is almost non-existent in civilized countries. When I mentioned infant botulism, she laughed and insisted diphtheria was the real cause and that Leah was extremely contagious. We all had to don masks and take precautions when handling her. This was long before Covid, and wearing a mask as I interacted with Leah just led to more frustration and desperation to find her cure.
Finally, a new doctor came on shift, and I begged for Leah to be tested for infant botulism. The only way to test for this bacteria is through the baby’s stool. However, the condition first attacks the muscles, so the baby no longer has bowel movements. Furthermore, the results take three days, and Leah was rapidly getting weaker. I knew from my research that the longer one waits to detect the disease the more havoc it wreaks, from attacking the muscles, to the nervous system, and then the lungs, until many such babies end up on respirators.
I was frantic. This doctor sensed my distress and agreed to come into the ward to see Leah. Upon seeing her condition, he declared, “This child is hypotonic with no gag or cough reflexes. She must go back to the PICU!”
Once back in the PICU, the staff began taking our situation more seriously. However, although they agreed to do a botulism test, they also insisted on doing a whole battery of other tests, including a spinal tap and EMG to rule out any other conditions. They sent me out of the room for the spinal tap, because it’s such a painful, horrible experience for the baby. But I was there to witness the many other tests they conducted on her, and each one pierced my heart, seeing my suffering baby subjected to more and more painful procedures.
When all the results came back negative, the staff finally admitted that botulism made the most sense. Despite the fact that the test results had yet to come back, they agreed to treat her for botulism. However, the only pharmaceutical company that made the treatment drug was in California, and the single dosage necessary costs $50,000, besides the transportation needed to get it to the East Coast.
With a marathon of phone calls, our insurance agreed to cover it, and Leah received her dosage even before she received the positive botulism test results. By the next morning, we already saw improvement: she opened her eyes and her mouth twitched into a slight smirk. I broke into sobs, feeling that there was finally light at the end of this tunnel.
The hospital set up a toy mobile above her crib. Although she still couldn’t move her head, they hoped the toys would stimulate her into action. By the following morning, her improvement was even more pronounced, and they decided to move her again to a regular ward. Yet this time, it was with the comforting reassurance, “She’s not going to get any worse. From here on, it will only get better.”
It was exactly a week since we’d entered the hospital. Despite my exhilaration at seeing her dramatic improvement, the staff warned me that we’d be transferring soon to rehab. Medically, she was on the road to recovery, but she’d need to relearn everything she’d been doing — turning over, sitting up, creeping, and most importantly, eating. Although she showed slight interest in nursing again, she still had no strength for the constant sucking, and that would be crucial to being able to take her home.
We moved into a rehab close to the hospital. It was a pretty, cheerful place with devoted staff, but many of the children were there long-term, and parents supporting their children were in short supply. It was so depressing to see these abandoned young kids. Also, in contrast to the hospital which had a fully supplied bikur cholim house with food and beds, the rehab had nothing to offer a frum family.
Shavuos was approaching, a three-day Yom Tov, and I was desperate to go home with Leah. The staff was skeptical, insisting we may need to stay for weeks, even months. But I was determined to take her home.
The main deterrent was her eating, and I spent hours with the feeding specialist patiently teaching Leah to nurse again. My husband and I both had to learn how to position the feeding tube and test its placement through a stethoscope, something squeamish I found difficult. But if this is what it took to bring Leah home, I was going to master it.
Erev Shavuos, exactly two weeks since Leah had gotten sick, we came home. The nissim and hashgachah that accompanied us throughout this ordeal were apparent in her quick release. Many children wait weeks for a diagnosis and treatment, leading to terrible decline and complications in their condition. I’m forever in awe of Hashem’s Hand in prompting my husband to tell my son’s morah about our baby and her quick connection to her niece.
Still, despite her rapid release, it took another six months of therapies until Leah was back to a full recovery. It wasn’t until after Succos we finally were zocheh to make a seudas hodaah, thanking Hashem for the miracle of this little princess.
What Is Infant Botulism?
Infant botulism (BAH-chuh-liz-im) is caused when a baby ingests toxins from Clostridium botulinum bacteria, which live in soil and dust, honey, and sometimes spoiled food. (In Leah’s case, the backyard soil was found to be contaminated.) That’s why babies younger than a year should never be given honey.
Babies who are affected by botulism are usually three weeks to six months old. Once the digestive system matures, the bacteria is harmless to older children and adults.
Signs and Symptoms:
>constipation (often the first sign parents notice)
>weak facial muscles that makes their face look “flat”
>a weak cry
>weak muscles in the arms, legs, and neck
>breathing problems
>trouble swallowing with a lot of drooling
>disinterest in feeding
>inactivity
Treatment ASAP
Doctors treat infant botulism with an antitoxin called botulism immune globulin intravenous (BIGIV), which neutralizes the toxins. This single-dosage treatment is made from pooled adult plasma from people who were immunized with pentavalent botulinum toxoid and displayed a high concentration of neutralizing antibodies. The faster this treatment is administered, the faster the recovery.
Still, experts don’t know why some infants get botulism while others don’t. And the only preventative guide given is the restriction of honey to young babies.
Information from Nemours Kids’ Health.org
My Mystery
My 10-year-old son constantly awakens at night and vomits. His stomach biopsies have all been clear, and his bloodwork shows IgA deficiency. He is also prone to migraines and he cannot read. Someone has suggested we try the GAP diet, but it seems impossibly difficult — yet I’m ready to do anything to help my suffering son. If any readers have possible insight, we’d be so grateful. Please email familyfirst@mishpacha.com.
(Originally featured in Family First, Issue 769)
Oops! We could not locate your form.