Deep and Dangerous
“I’m not hanging up until you tell me you’ll see a doctor today!” A mother’s intuition isn’t a small thing to ignore
As told to Faigy Peritzman
Being twenty-five years old and expecting your first child in a foreign country is a little overwhelming. Still, I was thrilled to have the zechus to give birth in Eretz Yisrael.
I started off using a private doctor, sure that this was the prudent thing to do with the Israeli socialized medicine setup. However, since my insurance only allowed a limited number of private visits, after a few uneventful months, I switched to a regular clinic doctor for the duration of the pregnancy.
In my last trimester, I started experiencing a heaviness in my right foot. It was an ache, a slight dragging feeling. I shared it with my doctor, who pooh-poohed it. “All pregnancies carry some degree of discomfort,” he said, waving his hand dismissively.
I took my lead from him and ignored it, despite the fact that the ache persisted for the next three months. I was sure it was just the baby pressing on a nerve, and after I’d given birth, I’d be fine.
Sure enough, the first week right after my son was born, I felt great.
My father came in for the bris and flew back two days later. I was on a high, but crashed a couple of days after he left. That Erev Shabbos I was talking to my mother in the States.
“You don’t sound good,” she said.
“I’m fine! I just had a baby,” I insisted.
“No, you really don’t sound good. You need to see a doctor.”
“Ma, it’s Erev Shabbos here in Eretz Yisrael.There are no doctors now.”
“You need to see a doctor now!” she insisted. “I’m not hanging up until you tell me you’ll see a doctor today!” A mother’s intuition isn’t a small thing to ignore.
What could I do? I promised I’d see a doctor, hung up, and then turned to my husband. “Where are we going to find a doctor now to make my mother happy?”
We tried a legendary frum doctor in our neighborhood, but he was unable to see us. He suggested I see a friend of his in a different area. Dr. S. kindly agreed to open his office for us half an hour before Shabbos. We dashed over there quickly. I just wanted to take care of my promise to my mother and get back home to light candles.
When I explained to Dr. S. that my leg and back were really hurting, he wasn’t too concerned, but since my mother had suffered from a deep vein thrombosis, he started me on a high dose of the anticoagulant Clexane/Lovenox on the spot and told me to go for an ultrasound on Sunday. I still didn’t believe this was my issue, since my mother’s blood clot had happened to her when she was in her forties. I was young with no other risk factors.
On Sunday I went for an ultrasound of my leg. There were some signs of a clot, but it didn’t look too bad, so they told me to just continue with my medication and sent me home.
A few days later it was clear the medicines weren’t working. I was a shmatteh, and could barely move to take care of the baby. Dr. S. sent me to the ER. He wrote a long handwritten note to explain the situation and requested a CT scan and Anti X — a blood test. It was a huge chesed that he took the time to do this, as the ER would have sent me right back home had he not.
When I arrived, they weren’t impressed with Dr. S.’s assessment. On the outside, they didn’t see any swelling, usually a tell tale sign of a clot.
One of the main diagnostic tests in an ER is based on the patient’s vital signs. But the danger of a blood clot is that vital signs remain stable — until they’re not. And at that point, it can be too late. The doctors in the ER were dismissive; they told me my heart rate was slightly off, but I was fine and could go home.
We fought them on this and insisted on a CT scan and a D-dimer test, which determines the levels of a protein your blood produces when there’s a blood clot. Finally, after hours, they did the CT. Immediately after the results came in, their attitude changed drastically.
Danger Zone
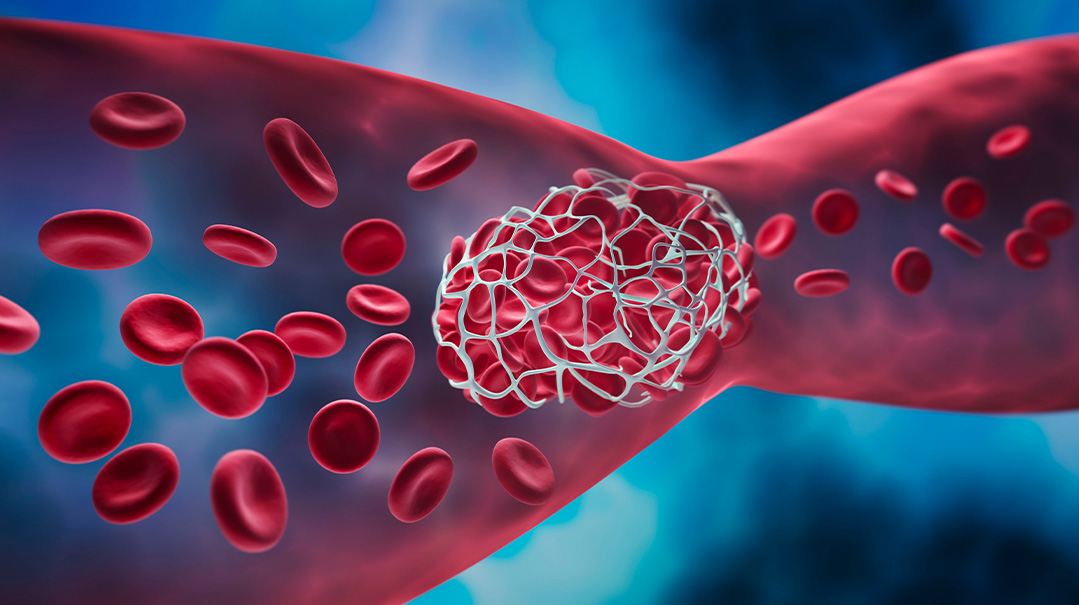
They had discovered a huge blood clot in my pelvis, an area they hadn’t bothered to check with the ultrasound the first time. Usually, if a clot is in the leg, you’d feel swelling to the touch and pain in the area, but mine was deep inside my pelvis, and there were no outward symptoms.
My clot was very high, close to my heart. It was a miracle it didn’t break off and go further up. One of the biggest dangers of blood clots is a pulmonary embolism (PE). This occurs when the blood clot breaks off and travels to the lungs, blocking blood from circulating through the body. This can be fatal.
Common signs of PE include shortness of breath or rapid breathing, sharp chest pain, rapid pulse, feeling faint or fainting, and coughing up blood. While I hadn’t had any of these symptoms, my blood clot was still in the PE danger zone.
Immediately, the hospital began doing blood work and adjusted my medication dosages. I was in the ER from Thursday night until Motzaei Shabbos. Sunday night was Rosh Hashanah. The hospital allowed me to go home for Rosh Hashanah, telling me to return afterward.
I went back early in the morning the day after Rosh Hashanah. Due to a miscommunication, I thought I was going to the hospital for a checkup, so I brought my newborn with me. I was surprised when they wanted to readmit me. I kept asking to see the doctor, but he was in a consultation. I later learned he was in a meeting about my case. Finally, hours later, the doctor came and said, “We’re doing surgery. Sign this paper.”
I couldn’t imagine why I needed surgery. My mother had never had such a procedure. But after more explanation, I realized how dangerous my situation was. Plus, it was clear the medications were not sufficing as I still wasn’t functioning well.
I was wheeled into surgery to perform a thrombolysis — a surgical procedure to open the vein to remove the clot. My surgery was a combined procedure that involved inserting a long tube to physically break down the clot and infuse medication to help with the process. Then, they needed to keep the vein open post-surgery in case they’d need to repeat the process, so the doctor inserted a stent — a metal mesh tube that expands against blocked or narrowed vein walls. It acts as a scaffold to keep veins open.
I was in the ICU for two nights to dissolve the clot with a clot buster, and on a high dosage of blood thinners so it shouldn’t clot again. All this time I had to lie flat on my back to keep the vein open. They had to continue the procedure after 24 hours to make sure there was no clot left.
Right after the procedure, I was in a haze, physically and emotionally, but I was grateful to Hashem that I’d made it this far. As time went on, I became more and more aware of the miracle that had happened and was thankful for just waking up each day. I felt indebted to Hashem for giving me such a wonderful family and a beautiful healthy baby.
I learned to appreciate the big and small chasadim that people did for me. Even small little things, like how those caring for my baby made sure he smelled clean and delicious for me.
After almost a week in the hospital, I was able to return home. Through subsequent genetic testing, I discovered that I have a genetic component, named Factor II, which causes my predisposition to blood clotting. This mutation means that my body makes more of the Factor II (prothrombin) protein than I need for normal clot formation, causing the risk of DVT.
My mother also has this factor, although she didn’t suffer from a DVT until she was in her forties. Still, although her condition manifested so differently from mine, she somehow sensed the urgency in my pain after birth. Her pushing me to see a doctor saved my life.
Baruch Hashem, I’ve since given birth to a second child, and still take blood thinners. As I know my risks, I’m careful to stay active and do yearly checkups with my hematologist, especially during pregnancy.
It’s crucial to be aware of your own body — what hurts and what doesn’t. Don’t listen if a doctor dismisses your pain. If something does bother you, check it out. Be aware, be educated, and you’ll protect yourself and your family.
What is deep vein thrombosis?
Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in the deep veins in the body, often in the legs.
Signs and Symptoms
Swelling in the affected leg. Rarely, there’s swelling in both legs.
Pain in the leg, similar to cramping or soreness.
Red or discolored skin on the leg.
A feeling of warmth in the affected leg.
DVT can also occur without noticeable symptoms.
Risk Factors
Sometimes, a blood clot can occur with no apparent underlying risk factor. This is called an unprovoked VTE. Generally, though, there are several common risk factors that can contribute to DVT:
Injury or surgery: The main causes of DVT are damage to a vein from surgery, trauma, or infection. Therefore, medication may be given to prevent clots before and after major surgery.
Bed rest: When your lower body is horizontal for long periods of time, the flow of blood slows and this can cause clots.
Long trips: When your legs remain still for hours, like on a plane or in a car, your muscles don’t contract; muscle contractions generally help the blood circulate.
Smoking: Tobacco usage adds to risk, especially when present with other factors.
Obesity: Extra weight increases the pressure in the veins of your pelvis and legs.
Pregnancy: The weight of a baby pressing on veins in the pelvis can slow blood circulation in the legs. Women with an inherited clotting disorder are at added risk. The risk from pregnancy can continue for up to six weeks after birth.
Hormonal treatments: Hormones in many treatments increase clotting factors in the blood.
Personal or family history: A previous clot or family members who’ve had clots puts you in a higher risk range.
Heart disease: People with heart disease may have limited heart and lung function and therefore even a small pulmonary embolism will be more significant.
Cancer: Some cancers, as well as some cancer treatments, increase blood clotting.
Disorders that affect clotting: Medical disorders such as kidney disease can also increase the risk.
COVID-19: People who have severe symptoms of COVID-19 are at increased risk.
Age: Being over 60 increases the risk of DVT, although a blood clot can occur at any age.
Bowel disease: Having Crohn’s Disease, colitis, or IBS increases the risk of clots.
Genetics: Some people inherit genetic risk factors, like Factor V Leiden, or Factor II, which make blood clot more easily.
Prevention
Avoid sitting still. During periods of bed rest, such as post-surgery, try to move as much as possible. While traveling, stop every hour to walk around, and don’t cross your legs while sitting. Exercises and stretches even while sitting also help.
Exercise and weight management: Regular exercise is essential, especially for people who are more sedentary.
Blood thinners (anticoagulants): These medications are often given before and after surgeries as well as to those at high risk.
Compression stockings: Compression stockings assist by squeezing gently, thus circulating the blood.
Leg elevation: Elevate your legs when sitting. At night, try propping up the bottom of the bed.
Hydration: Drink lots of fluids, preferably water. Avoid alcohol, which dehydrates.
(Originally featured in Family First, Issue 816)
Oops! We could not locate your form.