Safe Delivery
Was my golden tan a sign of something sinister?
As told to Faigy Peritzman by Shoshana Seif
When the pain hit on the right side of my ribcage, I almost doubled over. Collapsing on the couch, I gasped to my husband, “What’s going on? Was the salmon I ate at the kiddush spoiled?”
I could barely speak the pain was so bad. I’m not a complainer. Originally from San Antonio, I’m Texas-tough all around, and not one to take such pain sitting down, but this was incredibly intense.
I was in the middle of my fourth pregnancy, and from that day on, every time I ate fatty foods, the pain returned. I assumed it was my gall bladder, but an ultrasound showed no stones. As long as I avoided fats, I was pain-free, so I adjusted my diet and reached the end of my pregnancy attack-free.
In the delivery room the doctor declared, “You must’ve mistaken your due date. You’re way overdue. This placenta is very old, scarcely functioning.”
I was so glad to have my healthy baby girl, I didn’t pay much attention to him.
With a newborn and three little ones to care for, I reverted back to fatty food, and was grateful I could enjoy them pain-free. Assuming it had been one of those weird pregnancy quirks, I put it out of my mind.
My fifth pregnancy, two years later, started out calmly. That Succos, while in my eighth month, we went to the Kinar Hotel in the Galil with my in-laws. When we returned, I noticed I was very tanned. “I’m golden!” I said with pride. “Even my toes and fingers got tanned!”
But apparently, a tan wasn’t the only thing I picked up from the Kinar. That Friday night my palms and the soles of my feet started itching intensely. I ran to the kitchen, and using a Shabbos sponge, scrubbed my hands vigorously, but nothing seemed to ease the itching. I figured I’d caught a fungus from the hotel.
On Sunday, I called my labor coach, Barbara Perkal, for her advice on this nonstop itching. Barbara’s a registered nurse and certified midwife, as well as my guru. She knows everything there is to know about pregnancies, and I often consult with her.
She listened to my description carefully and then said, “There’s a rare condition called obstetric cholestasis that affects the liver during pregnancy. Best to go to your doctor tomorrow and check it out.”
“But my friend is making a bris tomorrow morning! Can it wait?”
“No, the condition can be fatal for the baby.”
With that dire warning, I dragged my itchy self over to my health clinic. Trying to remember what Barbara had described, I launched into a shpiel about my itchy liver. As hashgachah would have it, the head doctor of Hadassah Ein Kerem was visiting that day and they let me see him.
He took one look at me and asked, “Do you always glow?”
“Glow?” I repeated, picturing my kids’ glow-in-the dark stickers. “Oh, you mean my tan. Yeah, I tan easily.”
“You’re not tan,” he said brusquely, “you’re jaundiced. You need to go straight to the hospital.”
Hospital? This was not on my to-do list today. I still had dishes in the sink from Shabbos, laundry piled up, and I was zonked. All I wanted was to go home.
But the doctor was insistent. “Go to Shaare Zedek,” he said. “Ask for a bile acid test. They have the equipment to get results immediately, and time is of essence.”
“But I just had regular blood work done, and everything was fine.”
“Obstetric cholestasis doesn’t show up in regular tests. You must get this specific test.”
So, despite my reluctance, off to Share Zedek I went.
My sister-in-law came with me, and we sat there the whole afternoon waiting for the results as they ran a battery of tests.
Finally, when I thought it was either go home or bust, they said they wanted to admit me. My liver function test results were abnormal, and the bile acid test needed to be done first thing in the morning. “We may have to induce you,” they added.
Induce me in my eighth month? This was getting out of hand.
“What’s the big deal?” I wondered. “Why can’t I just come back tomorrow morning to do the test?”
There was a young doctor on shift and he agreed. “You’re right. It’s probably nothing. Besides, we’re never going to induce you before 37 weeks anyway. Go home and come back next Sunday when we generally do the bile acid test.”
Finally, a man after my own interests. Yet when he left, an older nurse approached me and whispered, “Don’t listen to him! This isn’t something you mess around with. You have to be proactive. I think you should be induced, but you didn’t hear it from me!”
How had I landed in this land of espionage?
I was so confused. My previous doctor had recently retired, and I didn’t have someone to consult with. Taking my chances, I dialed my old doctor on his cell. To my surprise, he answered, and after listening to my tale, told me firmly to get induced immediately.
So now I had one doctor who said come back in a week. Another who said give birth right now, and a nurse who was secretly supporting that approach. That nurse came back shortly with a number for a private doctor whom she said was excellent. I ran the name past Barbara, and she agreed.
With nothing/a lot to lose, I dialed him, and he answered. I was on the sixth floor in the high-risk ward, and he was on the ninth in delivery. He came down and listened to my whole story.
“You can go home now,” he decided, “but pay careful attention to the baby’s movements. If for any reason you don’t feel enough movement, come straight back!”
I went home and did my laundry. Relief. But I couldn’t relax. Some people were taking this seriously — and by then, so was I. I found out the hospital did the bile acid tests on Thursday morning as well. So early Thursday morning I was up at 4:30 a.m. to get to the hospital by 6:30 and do the bile acid test.
After I did the test, they sent me for a standard ultrasound. I’d been getting monitored every day so I wasn’t that worried. But the tech couldn’t detect any movement. She didn’t seem that concerned. “You probably didn’t eat or drink properly since you left the house so early. Go buy yourself a soda.”
I’m really careful with my sugar and… a soda? But hey, I followed instructions, drank, and went back. She tried again, but still couldn’t find movement. “You should probably get an ultrasound done by the specialist tech. He’s down the hall.”
Walking down the hall, I met the young resident from Monday. “Oh, you’re back? I told you, you didn’t have to come in until Sunday!”
So now I was in trouble for not listening to directions.
In the second ultrasound room, the technician asked, “What are you doing here?”
It was all too much. “I don’t know!” I started crying, and told him the whole story.
“You may have obstetric cholestasis and the tech can’t find movement and you’re just standing here? What are you waiting for?!”
I felt like answering, how should I know? I don’t work here!
“What are your results of the bile acid?”
“I just took it this morning.”
He logged into my account, but the results weren’t back yet. Yet as he went to log out, the results came in right then. Taking a look, he gasped. Over 10 micromoles per liter is problematic. My numbers were 46.
He started yelling about doctors and technicians who don’t know a medical emergency when they see one. I quickly dialed my new doctor who rushed me up to delivery to induce me. I was given extremely high levels of Pitocin, and baruch Hashem I was able to delivery naturally, without a C-section.
When the doctor delivered the placenta, there was absolute silence in the room. The placenta was black, disintegrated, full of holes, and completely non-functioning. Any longer, and the baby wouldn’t have made it. The doctor called in all the other doctors on call and showed them the placenta. “We should’ve taken this woman’s condition more seriously,” he admonished. Later, they offered me a formal apology from the department.
I was just thrilled we had our baby. We named her Elisheva Tova. Eli — as she was clearly here with yad Hashem, and sheva for the number that represents nature. Hashem had orchestrated the perfect sequence of events through nature that allowed it all to be tovah — good.
After Elisheva was born, I began researching my condition in earnest. I discovered that although the condition is called “rare,” it’s more accurate to say “undiagnosed.” It’s also probably one of the top causes of unexplained stillbirth. Since the bile levels revert immediately to normal upon delivery, there’s no way of determining if a stillborn was due to cholestasis. Yet, I found women all over the world who’d experienced what I had.
What was horrifying to me as well is they all experienced the same indifference and laissez-faire attitude when dealing with their obstetricians. One woman was a military wife and had three pregnancies with cholestasis in three different countries. She lost two of her babies due to doctors’ negligence.
Doctors claim that obstetric cholestasis is a silent disease — there’s no accompanying pain, and they insist that diet has no effect. Yet all the women affected insist that when eating fatty food, the pain, and even the itchiness, intensify.
Two years later, I was expecting my youngest. This time, my pain started in the sixteenth week. Again, I was very careful with my diet, adding fresh lemon juice, apple cider vinegar, and black beans — all good choices to combat the bile attacks. Still, I had one attack so bad that I ended up in the hospital. And once again, despite the fact I knew my own diagnosis and knew I needed a bile acid test, I was ignored and sent home with a prescription for an antacid.
By 36 weeks, I once again began experiencing the horrible itchiness. I went to the hospital and demanded a bile acid test. I wasn’t taking any risks with this child. They reluctantly gave me a test, but then told me my results were borderline, and I should go home. Of course my results were borderline: I’d been eating nothing but oatmeal for weeks! But I’d learned my lesson. I needed to be proactive to save my baby’s life.
“You need to induce me! Check your records and you’ll see that I had the exact same experience last pregnancy.”
The doctor remained stony-faced. “Our policy is that we don’t induce before 37 weeks,” he kept repeating as if reading from a textbook. “It’s not healthy for the baby.”
Not healthy! What wasn’t healthy when the baby may not live? With no choice, I went home, feeling helpless and panicky.
“You really should see Professor Grisaru,” suggested my friend Rena. “She’s head of Obstetrics in Share Zedek, and tomorrow she’s in the clinic in Geula.”
I was scheduled for a monitoring session the next morning in Geula anyway and begged the secretary to get me in to Professor Grisaru. B’chasdei Hashem, this time, I had the right shaliach.
Professor Grisaru was appalled. “They should never have released you to go home,” she said. She immediately wrote a strong letter with a referral for induction, signed it, and said, “Go straight to the hospital, they’ll induce you now.”
Yet when I got back to the hospital, they were annoyed I went behind their backs and told me I was thirteenth in line for induction. I’d have to wait my turn.
However, I soon began hemorrhaging and was quickly brought into delivery where baby Miriam was born safely, although her placenta, too, was already showing signs of damage.
When I look at my girls today, I’m awed by the chesed Hashem showed me in allowing them each to be born healthy despite the incredible danger they were facing. I realize, too, that my girls have forged me into being a better mother and person. Today, I’m a much more proactive parent than I used to be.
I’ve learned that you need to be your own advocate and to trust your knowledge of your own condition. It’s essential to find doctors who take you seriously and not give up when faced with dismissal.
Together with a close friend, I’ve also taken the experiences I had and used them to open a support group for women in my neighborhood who’ve experienced miscarriage or stillbirth. The group is called Not for Naught.
Because we all know it’s from Above.
What is Obstetric Cholestasis?
Obstetric cholestasis (kow·luh·stay·suhs) is a liver condition that occurs in late pregnancy. Pregnancy hormones rise as the due date approaches, and they slow the normal flow of bile — the digestive fluid made in the liver that helps your digestive system break down fats. Instead of leaving the liver, bile builds up in the organ. As a result, bile salts eventually enter the bloodstream, causing the following symptoms:
intense itching, usually on the hands and feet, but no rash
yellowing of the skin and whites of the eyes (jaundice)
nausea
loss of appetite
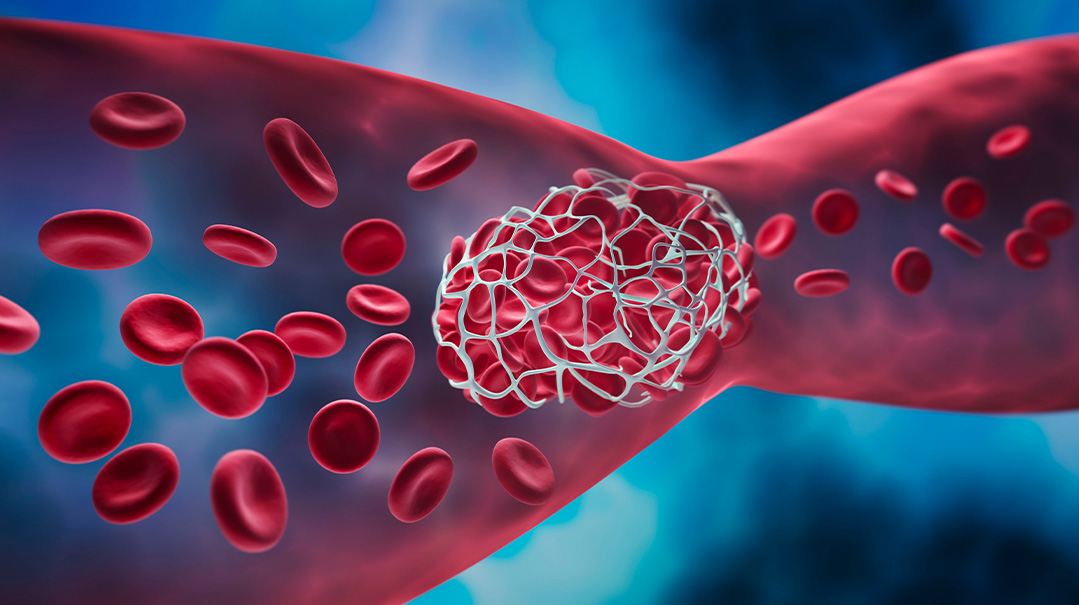
For the expectant mother, the condition may temporarily affect the way the body absorbs fat. Poor absorption of fat could result in decreased levels of vitamin K-dependent factors involved with blood clotting. But this complication is rare, and future liver problems are uncommon.
For the unborn baby, the complications of cholestasis of pregnancy can be severe. They may include:
pre-term birth
lung problems from breathing in meconium that usually collects in the fetus’s intestines but may pass into the amniotic fluid with cholestasis
stillbirth
Because these complications can be life threatening for the baby, inducing labor is often suggested.
Causes of cholestasis:
Genetics and family history of cholestasis of pregnancy
History of liver damage or disease
Multiple pregnancies
Previous obstetric cholestasis. 60 to 70 percent of women have a recurrence. In severe cases, the risk rises to 90 percent.
Information from the Mayo Clinic
(Originally featured in Family First, Issue 780)
Oops! We could not locate your form.