Painful Warnings

It was a simple case of COVID. So why was the pain off the charts?
As told to Rachael Lavon
My story begins as thousands of other did — at the end of March I came down with flu-like symptoms.
After checking in with my doctor and doing a swab, I was diagnosed with COVID-19 at the beginning of April. My options were limited in terms of in-person care, so the diagnosis of pneumonia was also made over the phone without the requisite X-ray.
As a busy mother in my early forties, I wasn’t considered a high-risk patient, but my doctor prescribed Zithromax and Plaquenil (also known as hydroxychloroquine) over the phone and told me to start taking them right away. I started the medication immediately as per my doctors’ instructions, but to my surprise I felt increasingly worse as the day wore on.
In the middle of the night I began having stomach pains and got up to use the bathroom. The next thing I knew, I was flat on the floor, my husband standing over me, looking scared. Apparently, I’d fainted and he heard the crash and came running. I felt totally disoriented while my husband helped me up then called Hatzalah.
By the time the Hatzalah volunteers arrived I was in a lot of pain, I told them I felt like I’d broken my ribs. They empathized with me and ordered an EKG to the house to make sure everything was okay. They also explained that the cocktail of medication I’d been taking was very strong and advised I switch to a different antibiotic. They EKG came out clear, and at last I went back to bed.
The next morning I woke up in absolute agony. I called my doctor again and explained that I really wasn’t feeling well.
“I’m in so much pain, I can barely move.” I whispered over the phone. “I really feel like my ribs are broken.”
“It’s completely normal to feel that way when you have both COVID and pneumonia,” the doctor said confidently.
Despite his assurances, a voice inside me was screaming that something was really wrong. Hatzalah members brought over an oxygen tank but even with that, my saturation numbers were low. I called a friend who’s a nurse practitioner and she urged me to get an X-ray as soon as possible.
We arranged for an X-ray to be done at home, but it was a long wait, and by the time we got the results, it was Erev Pesach, just hours before the Seder.
The results came back completely clear. My NP friend got the results directly and she called to tell me everything was fine. It was confusing for both of us; being that I was having so much trouble breathing, it seemed strange that my lungs looked so good. We were expecting to see signs of pneumonia on the X-ray at the very least. But there was no time for pondering the inexplicable as Pesach was hours away.
Throughout the first Seder I was in terrible pain and struggling to breathe. My extended family sent over huge amounts of food, but I couldn’t eat or do much of anything at all — it was impossible to find a comfortable position, I couldn’t even get in and out of bed, simply breathing took so much work.
At 12 a.m. on the night of the second Seder we heard an urgent knock at the door. My wonderful friend who’d helped me arrange the X-ray was standing there. I took one look at her face and knew something was very wrong.
“The X-ray service you used mixed up your X-ray with someone else’s,” she explained quickly. “You actually have a collapsed lung and need to go to the hospital immediately.”
I felt a mix of emotions rush over me. On one hand, everyone knew the situation in the hospitals was less than ideal. On the other hand, I’d been in terrible pain for days and at last my concerns were being addressed, there was a sense of relief.
Hatzalah kindly transported me to the hospital, they kindly gave me a big bag of food that had been prearranged, filled with matzos, Kiddush, and other staples. I was told I wouldn’t need to be there for long, so I hadn’t even thought to arrange a bag of essentials.
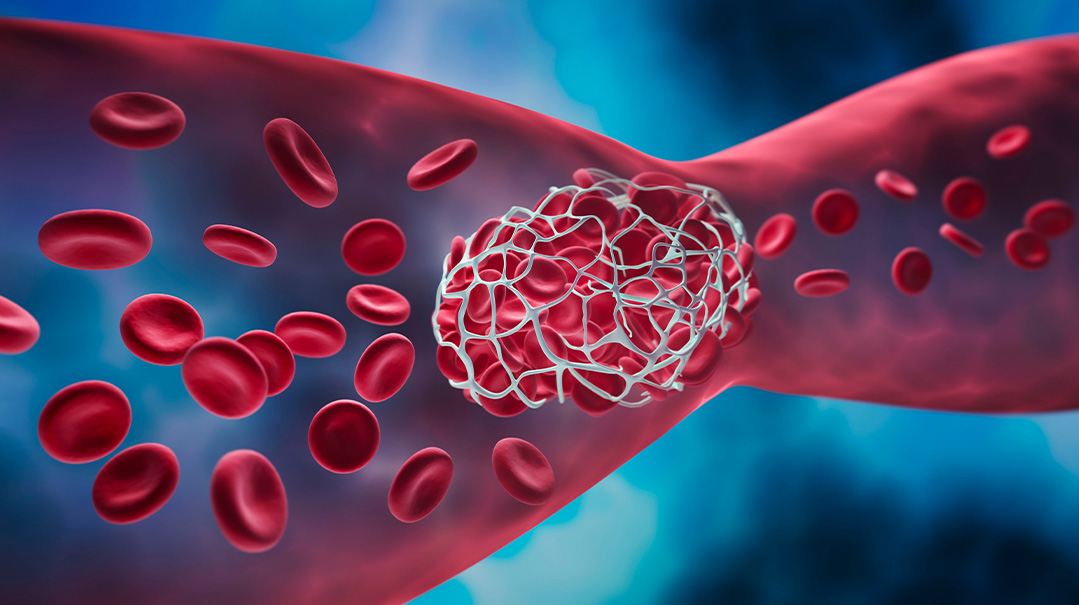
In the ER they did an X-ray that confirmed I had suffered from a pneumothorax. In order to reinflate the lung, they needed to insert a tube directly into the lung. I was fully awake during the procedure and it was exceedingly painful. The ER was a buzzing hive of activity with nurses, doctors, and patients everywhere, but despite the chaos, they took excellent care of me. I finally felt like I was getting the medial attention I needed.
After some time, they brought me up to a room and I expected the same attentive care, with a little more peace and quiet. However, the situation wasn’t quite like that. By now, everyone understands the difficult situation the hospitals were in over Pesach — they were full to capacity, but low on staff, as many of the nurses and doctors had just recovered from COVID themselves.
Getting in and out of all the protective gear necessary to enter the patients room was a time-consuming and tedious matter. Suffice it to say, there was no pressing a call button and poof, a nurse would appear. The nurses were very nice, they tried to do what they could under the circumstances, and I could tell that many of them wished they could do more — but it was simply impossible.
My roommate was having a very difficult time. She was going crazy stuck in the hospital room alone with no visitors and extremely limited personal attention. Her mental state immediately sent me spiraling; it was one thing to be sick, in pain, and stuck in the hospital over Pesach, and quite another having to share a room with someone who was in a disastrous mental state.
The hospital was also unequipped to handle our need for kosher l’Pesach food. I only received one kosher l’Pesach meal the whole time, though I was too sick to eat much at that point anyway.
During my stay in the hospital, I was in such excruciating pain that I could barely move. If circumstance had been different a nurse would have helped me to and from the bathroom as the tube in my lung and the unceasing pain made it very difficult to maneuver, but in this case, that was impossible. The nurses barely entered our rooms. The isolation was so thick, I can still feel it now, months later.
I made Kiddush alone with the grape juice Hatazala had given me, I closed my eyes and pictured my family. It was an extremely emotional time. The ward was filled with people but it felt like solitary confinement.
On Motzaei Yom Tov they finally took out the tube, and did a CT scan. I was still in horrible pain despite my lung doing better, and we finally found the reason: the CT scan showed that I had three broken ribs and a lacerated liver. My insistence that the pain was acute was finally validated. The liver healed quickly, but the ribs took a long time.
On Monday morning they told me I’d be discharged. I sat on the bed waiting all morning until around two p.m. when at last someone came to discharge me. They explained that unfortunately they were dealing with a difficult death, which caused the delay. It was a reminder of how blessed I was to be leaving the hospital healthier than when I came in and returning home to my family.
Back at home, I wasn’t expecting to feel fantastic within a week but I did expect an upward trajectory. However, as the days passed, I noticed I wasn’t getting better, I still couldn’t breathe. And oddly enough, my stomach and shoulder blade were hurting me tremendously.
I called the doctor and he told me he wasn’t concerned, he advised me to get plenty of rest and assured me I’d feel better in a few days. But I’d learned my lesson. I wasn’t going to ignore the pain. I went to an urgent care facility where they did an X-ray. They found a huge hiatal hernia pushing on my lung. It was so large, it could have caused a heart attack, chas v’shalom.
I spoke to a gastroenterologist as soon as I could, explaining the situation in its entirety. He told me not to worry about it, that he’d review my medical records and we’d discuss the situation in a few weeks when the medical system was back on track. I felt a little calmer after we spoke, but the next thing I knew the doctor called me back. This time, his tone was far more serious.
“I found your previous records. It looks like you had a tiny hiatal hernia before, but when you fell and broke your ribs, your stomach was pushed upwards and now 80 percent of your stomach is in your chest cavity.”
We sprang into action, finding the right surgeon who could fit me in within a short time span. At last, the surgery was scheduled for the day after Shavuos. Heading into the operating room, I was once again all alone, no family members were allowed to accompany me,it was just me and Hashem once again.
I woke up from the operation feeling awful. I was dry heaving from the pain medication (which only caused more pain) and I wasn’t allowed to eat or drink anything to settle my stomach. They had me do a swallow test the next morning to make sure the surgery was successful — unfortunately, they discovered that it wasn’t. I was informed that something had gone wrong and I’d need to go back into surgery as soon as they could do another CT scan. But the operating room suddenly became available and my situation was so dire that they skipped the CT scan and wheeled me into the OR just 15 minutes later.
Baruch Hashem, the second time around, the surgery was successful.
However, my story isn’t over. I don’t feel like I’ve recovered fully from my ordeal, my breathing is still strained, I have pain in places I never had pain in before, and I can’t eat the way I used to.
Yet my point in relaying my story is not to complain, rather to spur others into action. I’ve learned a huge lesson from this experience: pain should never be ignored. Hashem gave our brains the incredible ability to feel pain for a reason. While most doctors are sensitive and helpful, they still can’t feel what you feel. Please don’t ever let a doctor brush off your pain — listen to your body and find someone who takes your pain seriously enough to investigate its source.
(Originally featured in Family First, Issue 709)
Oops! We could not locate your form.