Out of Joint
It was just a stiff neck. Then it spread to my whole body

As told to Faigy Peritzman
I have a quirky personality; weird things just happen to me. Like when I lost my voice in camp. Normal, except my voice was nowhere to be found for months. Throughout 12th grade, I’d have my friends answer for me when the teachers took attendance.
I finally had a video endoscopy done, which showed that my vocal cords had no structural damage, so the ENT suggested vocal therapy. A few weeks in, my voice returned. Weird. But that was only the beginning.
A few days later I woke up with intense pain in my jaw — classic TMJ. We went to an oral surgeon and got an X-ray, which showed that nothing was wrong. The next day the pain had left my jaw, but it seemed to have relocated. I now had a major kink in the left side of my neck.
The sequence of issues with my voice, jaw, and now my neck was odd. But I could handle a stiff neck. I made sure to deal with it, because I’d be heading off to Israel for seminary in a couple of months. I went to a chiropractor and to a masseuse, but my neck was stubborn (they use the term stiff-necked for a reason!). I flew off to Israel with two oversized bags and a very stiff neck.
To keep the pain at bay, I arranged exercise classes in the dorm. I’d rally everyone to come and get moving, because I desperately needed the exercise to feel good. While my friends were concerned about the rockets falling on Yerushalayim, I was arranging to get to the chiropractor via taxi instead of bus.
I arrived home from seminary with renewed motivation to fix my neck before I’d fly off to camp in Atlanta. No such luck. I bought a microwavable beanbag that became my best friend. Other people need their cup of Joe first thing in the morning; I’d wake up, zap my beanbag, and find some small relief in the warmth against my aching neck.
Home again and then off to another camp, I found that wrapping scarves around my neck helped as well. Who cared that it was the summer? Since I lived in Canada, I decided I could pull off a scarf year-round.
September rolled around, and that’s when my neck pain went from bad to horrific. I had zero mobility in my neck and constant terrible migraines. I remember waking up at 4 a.m. and being unable to go back to sleep, pouring out my heart over Selichos.
My doctor booked me for an MRI, but with socialized medicine, I had to wait a couple months. Meanwhile, I was tying scarves around my head like a bandanna, which gave stability to my neck. I started doing acupuncture, experimented with pain meds, and bought all sorts of massage devices.
Lying down was really difficult. I had to cradle my head in my hands while lying down and getting up. Turning over in bed was an agonizing process, and I lived in constant fear of my head falling off.
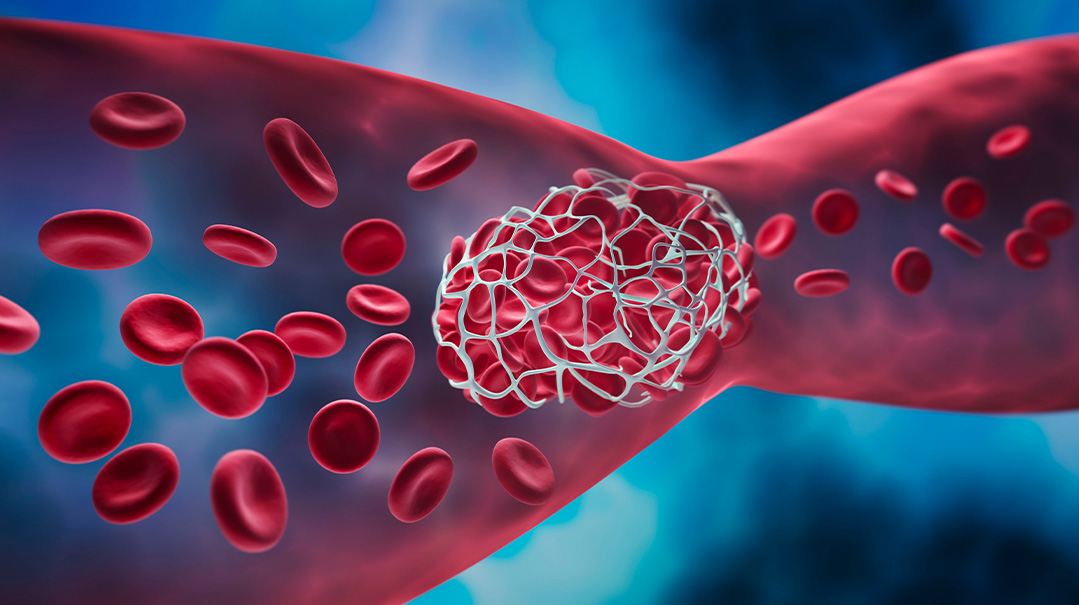
What I didn’t know at the time was that I already had an eight-millimeter (about of a third of an inch) subluxation between two of my vertebrae. A subluxation is a partial dislocation that happens when your vertebrae move out of position. Picture your vertebrae as a coil of rings — like a slinky — with your spinal cord running down the center. Now imagine if you’d pull one of the rings out to one side. Your finger would get squeezed by the rings. There was a large gap in my vertebrae, and my spinal cord had slid into that gap and was being compressed by the vertebrae, effectively limiting its functioning.
However, the radiologist who read my MRI completely missed this glaring issue — blatant medical malpractice. In hindsight, I should have insisted I receive the actual MRI imaging and brought it to all the specialists I consulted with, instead of relying on just the MRI report, which is the radiologist’s assessment of the MRI. But clearly Hashem thought I was cut out for more drama than that.
I was in a small frum college taking accelerated courses for a science degree. Classes were in the afternoons, so mornings were spent managing my neck. I went to a pain specialist, a specialized physical therapist, masseuse, and a restorative yoga clinic led by a guru who gave one-on-one sessions. All these helped me to manage the pain short term, but the months dragged on, and my condition was pitiful.
That whole year took on a surreal existence. My life was dysfunctional, but I was still studying chemistry until 2 a.m., shopping, even dating, and constantly begging all my family members for massages in between.
I pushed myself beyond what felt humanly possible because my MRI report showed that I was fine. I was in agony, but clearly there was nothing wrong with me, so life had to move on.
Having exhausted medical avenues, I began reading Dr. Sarno’s book on healing back pain holistically. I had a mantra that I’d repeat while putting my hand on my neck and forehead: “Subconscious mind, don’t give me physical pain instead of emotional pain.” I said it jokingly, but hoped that it would work.
I flew to Panama that summer on a SEED type of program. I shared my story of working to conquer pain with the girls there. When I returned, I started teaching, but my condition began deteriorating. I started to notice a slight tingling in my hands. I laughed it off to my friends as we walked together on Yom Tov. But at home in the chilly autumn night, it didn’t feel so funny. Something was very wrong, and I needed to get to the bottom of it.
Late one Motzaei Shabbos, I was experiencing numbness down both my arms. My father advised me to call a 24-hour nurse hotline. Hearing a rundown of my symptoms, the nurse instructed me to head to the emergency room. I laughed. I’d lived with this for two years; this could wait until the morning.
I took the subway bright and early and entered the ER. The resident there professed that I met diagnostic criteria for carpal tunnel syndrome, an issue in the wrists. But I had numbness and tingling all the way from my neck down to my fingers. This was clearly not a wrist issue.
I insisted that I needed another MRI. He refused. We negotiated, I got teary, and he gave in. Thanks to the ER visit, I only had to wait a week for the MRI. It was scheduled for the middle of the night. I wasn’t too hopeful. After all, I’d already had a perfect MRI a year before.
When we were done, the radiologist emerged, calling my name. He double-checked to make sure my name matched the person whose MRI he’d just assessed.
“Have you been in a car accident?” he asked.
“No!” I laughed. “I’ve just had a stiff neck for two years.” He looked at me like I was from Mars. Then he told me to follow up with my doctor.
As I awaited the results of the MRI, the numbness began spreading to my legs, and I was having a hard time keeping my balance. While teaching, I stopped writing on the board because my hands would shake so badly. If I dropped something, it just had to stay on the floor because I didn’t want to risk falling over to pick it up.
Due to more incompetence from the ER, it took a few days before my doctor called, distressed. “The MRI results are completely abnormal. You have an 18 mm (almost three-quarters of an inch) subluxation and need surgery right away!”
These are times when being a frum Yid has a lot of extra benefits. We contacted ECHO and Mrs. Botnick pulled strings to get us into a top surgeon. When he saw my MRI, he left me a message on Friday morning that I needed to get to the hospital immediately for emergency surgery. It was hard to believe that this couldn’t wait until after Shabbos, but we called a rav who yelled at us (kindly) to drop everything and get to the hospital — challah, grape juice, and all.
My father was still at work and met me in the ER. He walked back home on Shabbos morning to switch shifts with my mother. But before she arrived, the surgeon came in to meet me. He was shocked to see me standing in my Shabbos clothes by the window.
This doctor was as blunt as he was brilliant. “I’ve seen thousands of spines, but I’ve never seen such a huge gap in the vertebrae except on dead people. The only reason I can think of for you to have developed this problem is if you have rheumatoid arthritis, which is when the immune system attacks its own joints.
“The top two vertebrae act like a joint, and the inflammation around the joint makes the vertebrae move farther and farther apart, which then causes the spinal cord to become compressed. So, if you make it through this, you’ll have to see a rheumatologist.
“I must tell you, though, that you’re at risk for spontaneous death. Your breathing could be affected any moment because your spinal cord is so compressed. And as for the surgery, it’s going to be a bit of an experiment because we don’t know if it will be possible to fix such an extreme subluxation.”
There I was, 20 years old and alone, and I’d just been delivered a possible death sentence. But there was no alternative. Without surgery, my body was clearly shutting down. In fact, while I was lying in my hospital bed, I felt the tingling sensation take over my stomach. My body was now completely numb. Hashem would have to take care of me! I wished the doctor luck and gave my consent for the surgery.
Right after Shabbos, I called my friends to tell them what was going on. Like the near-teens we were, they came to the hospital, and I snuck downstairs for a pre-surgery party in the hospital coffee lounge.
The surgery lasted many hours as they needed to carefully screw my vertebrae back together with titanium screws. My mother describes how the surgeon came out dripping in sweat, looking like he’d run a marathon.
When I woke up, my neck was completely pain free for the first time in years. I was thrilled. But my euphoria was put on hold when I stopped breathing shortly afterward and had to be re-intubated. This was just temporary trauma to my airway, and I was breathing on my own 24 hours later. But the episode meant that I spent most of my time recovering as a VIP in the ICU.
With socialized medicine, it took months to get an appointment with a rheumatologist. During that time, my knees swelled tremendously with fluid, but the doctor wouldn’t drain it without the rheumatologist’s diagnosis. I’d gone back to teach in a neck brace, but now I could barely walk down the hall, let alone up the stairs. Once again, I was a mess.
Finally, I saw the rheumatologist and got my diagnosis of rheumatoid arthritis. Who would’ve imagined? I definitely didn’t have the classic disease presentation. I was young, had zero family history, and until recently the only joint that had been affected was my neck. For most people, rheumatoid arthritis is a manageable condition without serious risks. Developing a life-threatening condition like I did isn’t the norm.
Newly diagnosed and grappling with the idea of going on medication, I was advised that I’d be fine if I just worked on stress reduction. I decided to try reducing stress (who can argue with less stress?), but after some failed attempts at natural “remedies” and cutting out sugar and nightshades (don’t ask) from my diet, I accepted that I needed medication to get the inflammation in my joints under control.
I signed up for yoga and a mindfulness-based stress reduction course where I meditated together with my middle-aged friends who were undergoing various mid-life crises. But at the same time, I gave my rheumatologist the go-ahead to prescribe her best concoction of drugs. As much as I had suffered before this, something about the diagnosis and meds had been hard to digest, especially for a 20-year-old girl in shidduchim.
Thankfully, I now had my head screwed on straight and got over that hump.
As it turns out, there had been no need to worry, and I started dating my husband right around the time I was able to walk again. Chasdei Hashem, a few months later, I was able to dance at my own wedding!
Today I’m a busy mom of two and a registered dietitian. I thank Hashem constantly for keeping me alive and for the incredible blessings in my life.
Seeing me, you’d never know that my neck is screwed together and that I take drugs your doctor never heard of. The medication ensures that the inflammation in my joints stays controlled. I can tell when my medication is wearing off as I start to feel pain all over my body.
I still have close to zero mobility in my neck, although I compensate by moving my shoulders and torso so most people don’t notice. Occasionally, someone will ask me if I have a stiff neck, and it always makes me smile, because they don’t know the half of it!
In my work as a dietitian, I try to help people face their health with equanimity. I advocate for balanced eating, but I tell my clients to take their meds. And I teach them that they’re strong enough to deal with whatever life throws at them.
Did you ever have a medical problem that you were told “is nothing to worry about,” and it ended up being a serious issue? Did you have symptoms that stymied doctors? We believe sharing our journeys can bring awareness, empathy, and a sense of connection to those who’ve gone through a medical crisis. If you had a medical mystery and would like to be part of this column, please send a brief description of your story to familyfirst@mishpacha.com
What Is Rheumatoid Arthritis?
Rheumatoid arthritis is a chronic autoimmune disorder in which the immune system mistakenly attacks the body’s tissues. The inflammation associated with rheumatoid arthritis can damage other parts of the body as well.
Unlike the wear-and-tear damage of osteoarthritis, rheumatoid arthritis affects the lining of the joints, causing a painful swelling that can eventually result in bone erosion and joint deformity. The disease tends to affect smaller joints first — particularly the joints that attach the fingers and toes.
Signs and Symptoms:
Tender, warm, swollen joints.
Joint stiffness that is usually worse in the
mornings and after inactivity.
Fatigue, fever, and loss of appetite.
About 40 percent of people are affected in areas — besides the joints — that include:
Skin
Eyes
Lungs
Heart
Kidneys
Salivary glands
Nerve tissue
Bone marrow
Blood vessels
Rheumatoid arthritis signs and symptoms may vary in severity and may even come and go. Periods of increased disease activity, called flares, alternate with periods of relative remission — when the swelling and pain fade or disappear.
Over time, rheumatoid arthritis can cause joints to deform and shift out of place. Nonsteroidal anti-inflammatory drugs, steroidal medication, DMARDS, and biologics can reduce inflammation and pain and slow joint damage.
Information from the Mayo Clinic
(Originally featured in Family First, Issue 774)
Oops! We could not locate your form.