New Brother, Old Brother

The brother we knew was never coming back

One winter day six-and-a-half years ago, I was driving down the Garden State Parkway in a storm of freezing rain, traveling with my parents from Brooklyn to Lakewood for a relative’s bris.
My hands were clenched on the steering wheel, and I was driving slowly and very carefully, due to the weather conditions, when we passed a slew of emergency vehicles at the site of an accident. With a silent tefillah that no Yid should be harmed, we continued on our way.
About five minutes later, my mother’s cell phone rang, and a few moments after she answered, she slapped her leg really hard.
My first thought was: Oh, no! Did we forget the bris outfit?
For a while my mother could not talk, but finally she blurted out, “Yanky and Avi were in a bad car accident.”
I immediately pulled over to the shoulder of the highway.
“Yanky will be okay, Tzippy,” she continued, clutching the armrest. “But Avi” — her voice dropped to a raspy whisper — “Avi is unconscious.”
“People lose consciousness all the time, and then they recover,” I assured her.
But in my own mind I was already carrying on a very different dialogue with Hashem. Please don’t take Avi away from us, I begged silently. Let him have a full recovery. Please, please don’t let there be any long-term negative effects.
Avi was the youngest in the family, ten years my junior, and from the moment he was born, he was the biggest brachah to our family. A delightful child, he quickly earned a special place in everyone’s heart, and as he grew older, his many gifts became increasingly apparent: He was blessed with a winning personality, a kind and giving nature, a bright mind, and a great sense of humor, and he was good-looking and athletic, to boot.
A hardworking eleventh-grader, Avi would rise each morning at 6 a.m. to learn with his chavrusa in shul, after which he would head to yeshivah to learn. At night, after seder, he would relax by playing basketball with his friends. Any task that had to get done, he was happy to do; when he built our succah, playing lively music as he worked, the whole family invariably congregated around him, because it was so much fun to be in his presence.
He was also exceptionally sensitive to other people’s feelings. Once, he went on a skiing trip with his friends, and when he returned, I asked him whether he had braved the most challenging slope. “No,” he said.
“Why not?” I asked in surprise.
“Because I saw that one of my friends was scared to do that slope, and I didn’t want him to be embarrassed, so I told him I didn’t want to do it, either.”
Avi’s rebbeim loved him and would frequently call “just to give some nachas.” When my father would walk to shul with him on Shabbos, his face would beam with pride.
I couldn’t bear the thought of my baby brother being any different from the way I knew him. My mind jumped to the worst-case scenario: What if this turned out to be a life-altering injury? We could not handle that.
As these thoughts swirled around in my head, I called my sister to tell her we wouldn’t be making it to the bris, and replaced our destination in Waze with “Jersey Shore Hospital.”
When we arrived at the hospital, we were told that the staff was working on Avi and that we could not go in to see him yet. We were able to go in and see my other brother Yanky, who looked like he had emerged from a war zone: His whole body was bruised and battered, and he had stitches in multiple places and several broken bones. He had suffered a concussion and had no recollection of the accident. But he had escaped serious injury, and the doctors assured us that he would be fine.
Avi was a different story. After about an hour, a tall, thin doctor emerged, a grave expression on his face.
“Right now he is hovering between life and death,” he informed us.
My mother and I immediately experienced an intense wave of nausea, and we bolted for the nearest restroom.
Finally, we were allowed to go see Avi, who was hooked up to innumerable tubes, wires, and machines. Remarkably, unlike Yanky, Avi did not have a single scratch on his body.
While to this day we don’t know exactly what happened, it appears that due to the inclement weather, their car skidded off the road, flipped over twice in the air, and collided with a large road sign on Avi’s side. Because he was wearing a seatbelt, he remained anchored in place throughout, and his brain shook forcefully against his skull — a form of “closed-head” traumatic brain injury known as diffuse axonal injury. Avi also had many broken bones as well as other internal injuries.
The accident was reported on frum and general news outlets, so people throughout the Jewish world learned about Avi’s condition very quickly. I remember thinking how bizarre it was that our family was being featured on the news — I had always assumed that the disasters reported in the media happened to other people. I couldn’t come to terms with the idea that this was happening to us.
The next day, a doctor came to speak with my mother.
“I wish you the best outcome,” he said, “but one thing is for sure — if your son survives, he’s never going to be the same. Your son, as you knew him, is never coming back.”
“How dare he say that?” I fumed, when my mother reported his words to me.
That evening, some family members and I were discussing what the doctor had meant when he said that Avi would never be the same. One sibling speculated that perhaps the doctor meant that Avi would be left with a speech impediment.
Avi, a speech impediment? We were horrified by the thought.
“Maybe he’ll be left with a limp,” another family member suggested.
That thought was equally horrific. We couldn’t even imagine Avi’s tall, strapping figure nursing a limp.
“The doctors are so arrogant,” we all agreed. “They don’t know anything. It’s all in Hashem’s hands.”
In hindsight, I recognize that we were all in a state of denial. We simply could not accept, at that point, that the old Avi was no more. At the same time, the doctors themselves were unsure of Avi’s prognosis.
“The brain is a very complex and poorly understood organ,” they told us. “There’s no way to predict what the outcome will be.”
In the days after the accident, many other family members and I were spending much of our time in the hospital, barely eating or sleeping. Yet there was nothing we could do for Avi at that point; we were not even allowed to speak to him, since the medical staff warned us that speaking to him could lead to increased brain activity, which could cause additional swelling.
“After three days the swelling will start to go down,” they said. “Then you can talk to him.”
We naively assumed that this meant that after 72 hours we could carry on a regular conversation with Avi, and he would talk back.
To our shock and horror, when we were finally allowed to speak to him, it was like talking to the wall. When my mother lifted his hand, it felt like dead weight.
The one encouraging sign was that when my mother started talking to Avi, the machines started beeping loudly. A nurse ran into the room to see what was wrong, and she explained that his blood pressure had risen. That meant that Avi was able to hear — and to recognize my mother’s voice.
Still, the doctors were very pessimistic, telling us that on the coma scale — a measure used to assess a person’s level of consciousness after a brain injury — Avi was just one step removed from brain dead. They knew there was no chance Avi was going to respond to us anytime soon.
We, however, were sure that Avi was going to awaken any moment. Each time I spoke to my parents or siblings, the conversation went something like this:
“Did he respond yet?”
“No.”
“Okay, so hopefully he’ll respond tonight. Or maybe in an hour.”
Living as we were with the feeling that at any moment something was going to change, we could hardly think of anything besides Avi.
One night, a few days after the accident, I left the hospital to finally sleep in my own bed, and I returned home to find the kitchen table full of food that caring neighbors and friends had brought over. One cousin had sent a tray of delicious chocolate chip cookies, and while I should have been hungry enough to devour the entire batch — I hadn’t put anything into my mouth all day — I had to force myself to pick up a cookie and take a bite. But I felt so nauseated that I couldn’t even finish the cookie.
In the meantime, Avi was transferred to the ICU at Manhattan’s Columbia Hospital, where he remained for the next two months. One Shabbos, when I went to visit a patient who was hospitalized on bed rest and found her all alone, she told me that some weeks her mother came to spend Shabbos with her but would not leave the room the entire time, for fear of being mechallel Shabbos by activating an electronic door.
We, too, encountered questions of this nature all the time, and we realized that people accompanying their loved ones in the hospital were forced to be either too lenient or too stringent about observing halachah in that setting. Often, we expressed the wish that there were a pamphlet addressing common halachic questions that arise in the hospital.
About six weeks after the accident, we noticed that Avi was starting to blink his eyes, and we became very excited.
“He’s starting to respond!” we told the doctors.
“No,” they said. “That’s just a sign that he’s experiencing sleep-wake cycles. That typically happens about four to six weeks after a brain injury, but it’s not a sign of responsivity, and it certainly does not mean he’s regaining consciousness.”
Hearing this, I felt as though I had been slapped in the face.
Two and a half months after the accident, my mother shared a dilemma with me. “Every morning I wake up thinking Avi will definitely respond today, and then he doesn’t. Should I continue hoping and being disappointed, or should I just give up — and then, when it finally happens, I’ll be pleasantly surprised?”
The next day, she told me that she had resolved the dilemma.
“I decided that I have to keep on hoping,” she said.
Avi’s recovery — if it could be called that — was excruciatingly slow, with frequent regressions. Once, the medical staff determined that he could finally be extubated, but then he experienced a crisis, and needed to be reintubated immediately.
I had always thought that a coma was a peaceful state, similar to sleep. But that was hardly the case with Avi. Much of the time, he was clearly agitated, thrashing about, grimacing, and obviously in pain. To restrain his uncontrolled, spastic movements, he had to be seat-belted into his bed.
Seeing him in this state was simply unbearable.
“Please, Hashem,” I begged, “just take him! We can handle losing Avi — we’ll be sad, but we’ll move on. But we can’t keep seeing him like this.”
After two months, with Avi still unresponsive, the staff at Columbia started talking about transferring him to a rehab center. In our minds, rehab meant that Avi was ready to relearn how to walk and speak, but the doctors quickly dispelled that notion.
“Maybe they’ll manage to teach him to sit up in a wheelchair,” they said. “He might even learn how to smile.”
Before Avi left Columbia, the staff decided to try sitting him up. As three physical therapists strained to lift him to a sitting position, my mother and I prepared ourselves to speak to him; for some reason, we assumed — quite irrationally — that as soon as he was sitting up, we would be able to communicate with him. When he was finally propped into a sitting position, he looked dead — a lot more dead than he had appeared while lying down, when he could have been mistaken for a sleeping person.
Upon seeing his vacant face opposite us, my mother ran to the restroom, while I lunged for the nearest chair, feeling faint. The physical therapists looked confused: A minute ago the two of us had been preparing to talk to Avi, and now we were both gone!
We expected rehab to work magic on Avi, but instead, the therapy he received focused on the most basic of functions, such as teaching him how to swallow and how to sit in a wheelchair.
Because he had not exercised in months, his muscles had atrophied, causing his limbs to stiffen and remain frozen in unnatural positions. (Eventually, he would undergo several surgeries to repair this.) One image of him remains frozen in my memory: His head was bent to the side, practically touching his shoulder; his mouth was drooling nonstop; a feeding tube was threaded into his nose; his right leg jutted out straight ahead; and his entire body was shaking in agitation.
I’ve seen plenty of children with special needs, I thought. But I’ve never in my life seen a person look this bad.
When the therapists informed my parents that Avi would need a back brace to help him sit in a wheelchair, they gave her a choice of flashy colors for the brace, as appropriate for a typical teenager.
“My son wears a white shirt and black pants,” she told them, “so he needs something more conservative than what you’re showing me.”
Ma, I thought sadly, he’s never going back to wearing a white shirt.
The contrast between our memory of Avi the yeshivah bochur and the reality of what Avi was today could not have been more stark. Yet despite his depressing prognosis, our family persisted in doing every possible hishtadlus, both spiritually and medically.
On the spiritual front, we had all our tefillin and mezuzahs checked, we joined Tehillim groups, we increased our giving of tzedakah, and we sponsored countless learning programs as a zechus for Avi. We arranged chavrusa partnerships for women to learn a sefer about tzniyus, and we divided the Shemoneh Esreh among our family members, with each person committing to have extra kavanah in a particular brachah. Three of my siblings flew to Eretz Yisrael to daven at mekomos hakedoshim and get brachos from the gedolei hador.
Besides our family’s kabbalos, relatives, friends, and neighbors all rallied to amass zechusim for Avi as well. Three daily Tehillim groups were arranged by dedicated neighbors and a close friend, while biweekly shiurim were organized by another family friend. Avi’s yeshivah instituted a new seder in shemiras halashon after Shacharis every morning, which continues to this day. We felt like we were being carried by the klal, and we were confident that through everyone coming together, we would surely merit the miracle we so badly needed.
On the medical front, with the help of amazing Jewish organizations and askanim, we did nonstop research into any possible option for Avi’s recovery, conventional or otherwise. We contacted every medical advocate whose name we heard, and explored any and every avenue that was suggested, investigating one rehab center after another to see whether Avi could receive better therapies there.
Although we are hardly believers in alternative medicine, we brought in various practitioners who thought they could help Avi, even if their methods seemed wacky. If there was the remotest chance that something could help, we did it.
Still, the doctors would come into Avi’s room every day and shake their heads sadly.
“You have other children,” one doctor told my mother, about five months after the accident. “Put your son in a long-term care facility, and go home and enjoy the rest of your family.”
By this time, Avi’s time in rehab had run out, and my parents had to decide what to do with him. Should they bring him home and create a hospital-like environment in our house to accommodate him, or should they follow the doctor’s recommendation and place him in a long-term care facility — a nursing home, for all practical purposes?
Neither of these options appealed to us. We wanted Avi to continue receiving intensive therapy, and that would be possible only in an acute rehab facility. We even found the facility that we thought was right for Avi: the Kessler Institute in New Jersey. We were told, however, that our insurance would cover only a long-term care facility, considering that Avi had already spent two months in acute rehab without progress.
BINA, the remarkable frum organization that helps victims of brain injury and their families, had been supporting our family since right after the accident, and we turned to them again to help us get Avi into Kessler.
“In the history of our organization,” the people at BINA told us, “we have never heard of a patient who went to two acute rehab centers. For one thing, insurance will not cover a second stint of acute rehab, and for another, if a patient did not make progress in one acute rehab center, why would a second rehab center take him?”
“We’re ready to pay out of pocket,” my father assured them. “I’ll mortgage my house, if necessary.”
“It doesn’t work like that,” they explained. “These rehab centers only accept patients with insurance. You can’t pay privately even if you want to.”
My father would not give up, though. He wrote letters to every politician who he thought could exert some influence, and prevailed on countless prominent individuals and askanim to help get Avi into Kessler.
To BINA’s credit, they did their utmost to help us, even though they thought our efforts were futile. My siblings and I also thought my father was wasting his time, and we felt bad for him, knowing he had hardly any chance of succeeding. In the end, however, with the help of a caring US senator, Kessler agreed to accept Avi. Miraculously, by a fluke, it appeared that insurance had agreed to cover the bill. There was a mistake in the paperwork, and Avi was approved — erroneously, it turned out — for a second acute rehab stay. (In a remarkable and unprecedented development, Kessler ultimately accepted the blame for its misunderstanding with the insurance company and agreed to absorb the loss.)
The final requirement for Avi to be transferred to Kessler was the recommendation of his current doctor that he be sent there.
When my mother requested such a letter, the doctor looked at her with sad, pitying eyes and said, “You’re chasing a magic bullet that doesn’t exist. But I won’t stop you.”
The fact that Kessler agreed to take Avi infused us with renewed hope, because that meant they thought they could help him. And indeed, the attitude there was completely different from that of the first rehab center; they actually believed they could get him to respond.
For the first six weeks of Avi’s stay at Kessler, we saw almost no progress. The only improvement was that his eyes were perhaps starting to follow people.
To prepare Avi to learn how to walk, they casted his legs into the correct position and began training him to put weight on his legs — but to no avail.
One day, Avi suddenly began to utter deep, guttural moaning and groaning sounds. This was the first time, since the accident, that he had performed any vocalization — which would have been a positive development, except that it came along with foaming at the mouth, thrashing, shaking, and eye-rolling. Seeing that Avi was obviously agitated and in terrible pain, we begged the medical staff to give him sedatives and painkillers, but no amount of pain medication seemed to give him relief, and seeing him in that state was indescribably torturous.
One Sunday, when my mother was with him, he finally quieted down. Thinking that he had fallen asleep, she began saying Tehillim in her chair, grateful that he was asleep and no longer as miserable. But then she looked up and saw that his face was white and his lips were blue.
She quickly summoned a nurse, who could not find a pulse. Avi was in cardiac arrest.
The doctors worked for 20 minutes to resuscitate him, after which he was rushed to the nearest hospital, St. Barnabas, where he was placed on maximum life support.
Doubtful that he would make it through the night, the doctors instructed the family to say our goodbyes. As we raced to St. Barnabas, my father contacted one of Rav Chaim Kanievsky’s gabbaim, who described the situation to Rav Chaim and relayed to us his instruction to add the name “Refoel” immediately, in the car — even without a minyan. By the morning, baruch Hashem, Avi’s condition had somewhat stabilized.
“Avi’s body just needed to reset,” my mother kept saying. “Now he’s going to start responding. This setback was a blessing in disguise.”
My heart ached to see her in such denial. Whereas Avi had been breathing on his own before, now he was connected to a trach, and the doctors didn’t expect him to ever be weaned off it, considering that his lungs had sustained serious damage. They also thought his leg would need to be amputated.
While we had thought many times that we had hit rock bottom, this time we were shocked yet again to discover a new rock bottom. How much can this poor, innocent boy suffer? I wondered tearfully.
“It’s so sad,” I told my sister one day. “Avi died, but there’s no shivah, so we don’t have the comfort and closure that comes with it.”
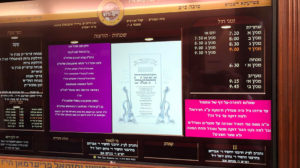
At this point, my family arranged a conference call, realizing that we had to do something huge as a zechus for Avi — now Refoel Avraham. As people in the family kept rehashing old ideas — shemiras halashon, tzniyus, Tehillim — I suggested a brand-new concept: to prepare a pamphlet of questions and answers addressing common halachic issues that arise in the hospital.
“Let’s get answers from rabbanim and distribute those answers to Bikur Cholim rooms in various hospitals,” I said.
Everyone loved the idea: It was different, it was practical, and it was meaningful. Until this point, we ourselves had called rabbanim after every Shabbos in the hospital to ask the questions whose answers we had needed to know over the course of that Shabbos. Now, people would be spared that added difficulty of not knowing what to do while in the hospital, as they would have the answers prepared for them.
Two of my brothers are well-versed in halachah, and while the rest of us prepared the questions, they set out to research the answers. For many months afterward, they studied the relevant halachos, consulted with rabbanim, and wrote up the answers to the questions we had prepared. Eventually, what started as a little pamphlet turned into a full sefer, which my brothers brought to leading poskim for review.
In the meantime, Avi had been discharged from St. Barnabas back to Kessler, but his condition was far worse than before, and he was given an 8 percent chance of regaining consciousness. By now, our hopes for him were pathetically minimal: “If only he would learn to sit up.” “If only he would be able to blink yes or no.” “If only he would show some recognition when people visit.”
When people would ask for a report on Avi, we didn’t know what to answer. “Yeah, the situation is difficult, yeah, there’s no progress, but yeah, keep davening,” we would say. “Who knows?”
One friend of my mother’s heard this and responded, “We’re going to continue fighting! A Yid never gives up.”
A month after Avi’s return to Kessler, he was weaned off the trach, even though the doctors had said he’d be on it for life.
Then, one day, my mother called me from Kessler, and when I picked up, she promptly started to cry.
What now? I thought, my heart sinking.
“I think Avi may have responded.”
Apparently, the therapist had instructed Avi to raise his hand — and he had complied!
“Is it fair to be hopeful, Tzippy?” my mother asked anxiously. “I’m so scared to get my hopes up again!”
The therapists began placing a big buzzer in front of Avi and telling him to press the button — and he started leaning forward to touch the buzzer. His movements at this point were jerky and uncoordinated, but he was definitely responding.
From there, things started happening in all areas of development. Avi learned how to sit up and how to eat.
Once, when I left his room Friday afternoon, I said, “Bye, Avi, have a good Shabbos.”
He mouthed back to me, “Have a good Shabbos.”
After that he continued to mouth words with his lips — not vocalizing and not saying words of his own, just repeating what other people had said. But soon, he started mouthing his own words, and even saying brachos.
At this point, the people at Kessler started touting Avi as their big success story. Once, a staff member was giving someone a tour of the facility, and they stopped in Avi’s room and said, “This kid is responding after being unconscious for eight and a half months — and a big part of that is because he has devoted family members, relatives, and friends who are with him 24-7.”
In addition to Avi’s official physical therapy sessions, other family members and I would practice his walking with him. His progress, while remarkable, was agonizingly slow, as he had to relearn everything.
After six months, Avi was discharged from Kessler to a subacute rehab facility. By the time he left that facility, six months later, he was able to walk out on his own, using a walker. He had relearned how to speak, albeit in a whisper and without inflection, and was able to recognize and communicate with the people around him.
His return home, alive and aware, was nothing short of a miracle.
It was also very bittersweet. The Avi who came home to us was nothing like the Avi who set out for that family simchah a year and a half earlier. He was severely disabled in every way: physically, verbally, cognitively, motorically, and otherwise.
Today, six and a half years after the accident, Avi has almost no short-term memory and doesn’t remember what he did five minutes ago. His balance is poor, and he needs someone to hold his hand when he walks to ensure that he doesn’t fall — but because he doesn’t remember that he has a tendency to fall, he persists in trying to walk on his own and hurts himself very often. He still goes for therapy and attends a “day-hab” every weekday.
Avi does not have much capacity for high-level thought nor can he engage in meaningful conversation. Yet at the same time, he is joyful and content, and is deeply connected to Hashem. He loves to learn Torah and daven and is constantly seeking to do chesed for others. Mitzvos are of utmost importance to him. He also has a great sense of humor and often makes for very pleasant company.
When Avi was unconscious, I thought that if he recovered with severe limitations, or with an altered personality, I would not be able to relate to him; I was sure that every time I looked at him, I would burst out crying. But even though he’s not who he used to be, my family members and I do not find ourselves constantly comparing him to the old Avi.
Occasionally, memories of the old Avi are triggered, such as when we receive invitations to his friends’ weddings, and at those times we feel sad. But overall, we’ve made peace with the new reality, and we’ve moved on.
Torturous as it was to see Avi in a coma for months on end and suffering terribly, we are all so grateful to Hashem for returning him to us, even in his compromised state.
I realize now that what makes a person alive is not his personality, or his intelligence, or his abilities — it’s his neshamah. Avi’s neshamah is the same now as it was before the accident, and because that’s the part of him that we connect to, we no longer feel that the old Avi died, even if his cognition is at a three-year-old level in many respects.
Six months after Avi’s return home, we made a seudah in honor of the publication of Hospitals in Halacha: A Practical Guide for Visitors. This sefer was truly a family endeavor: My brothers wrote it, my parents sponsored it, and other family members edited, designed, and oversaw its publication and distribution. Even Avi took part in the effort, affixing the labels that said, “Please return to the Bikur Cholim room.”
The sefer, to us, is a lasting legacy of Avi’s accident. More than anything, it expresses the idea that we are here in this world to do Hashem’s will under any and all circumstances and that we recognize that whatever happens to us is what’s meant to be — and what’s best for us.
In the meantime, Avi keeps us entertained with his witty comments. At the Shabbos table, he’ll say, “Deliver the liver,” or ask someone to pass him the “Polisher vasser,” a reference to Poland Spring water. While he’s not the same Avi he used to be, his place at the table is still full, and for that we’re forever grateful. —
The newly revised and expanded sefer, Hospitals in Halacha: A Practical Guide for Visitors is now available in local Judaica stores. A downloadable version is available at
www.tefillahnetwork.org.
The narrator and her family may be contacted through LifeLines or the Mishpacha office.
To have your story retold by C. Saphir, e-mail a brief synopsis to lifelines@mishpacha.com or call +1.718.686.9339 extension 87204 and leave a message. Details will be changed to assure confidentiality.
(Originally featured in Mishpacha, Issue 876)
Oops! We could not locate your form.