Hidden Growth
I tried it all: diets, medication, therapies. But nothing relieved the pain

As told to Faigy Peritzman
Y
ou don’t know me, but I’m a very polite and respectful person. Standing up for myself isn’t my strong point. I was raised to think that people in the medical field know it all, and if a doctor says something, you do as he suggests because he knows best.
But I’ve learned the hard way that this doesn’t always work.
As a teen, I was diagnosed with Irritable Bowel Syndrome. By the time I reached high school, I was in the borderline gray zone for Inflammatory Bowel Disease, with some complications that needed to be taken care of surgically.
Thus began a very long medical journey.
I live in Canada where there’s universal healthcare. There are long waiting lists to be seen by a specialist. In my case, I even had to deal with personal issues between two medical professionals (who shared offices in the same building), who would let out their frustrations on me, the patient stuck in the middle. One even told me, “Go back to Dr. So and So. He got you into this mess.” Subjected to such ridiculous byplays affected my health and overall wellbeing.
A few months after graduating high-school, I experienced the culture shock of transitioning from the children’s hospital to the adult hospital where the care and nursing ratio was very different. My pediatric gastroenterologist referred me to a colorectal surgeon.
Just a few months earlier, at the children’s hospital, the staff surgeon of the gastroenterology team tried to avoid subjecting me to surgery by performing a non-invasive surgical procedure — sclerotherapy injections into my intestines — but they left me with long-term nerve and muscle damage.
At the consultation in the adult hospital, the colorectal surgeon informed me that the procedure I’d undergone is actually one designated for toddlers, whose muscles are still developing, and that after that age, it’s considered to be harmful. In her words, “They botched you up.”
She recommended intestinal surgery to fix things. My parents and I agreed to surgery, as this seemed to be the only option. Now, looking back on how things began, there were probably many more, less invasive ways to fix my gastrointestinal problems earlier on, before undergoing the procedure that left me with no choice but to now undergo major surgery.
To complicate matters, the surgeon decided to do a full open surgery instead of the usual laparoscopic method. To this day, I have no idea why. Was it more convenient for her? Lucrative? Was I not worth an extra hour or two in the operating room?
Whatever the case, I woke up with a host of complications from the open surgery. Immediately afterwards I contracted Clostridium difficile (C. diff), a bacterium that causes an infection of the large intestine (colon) and can cause colitis, an inflammation of the colon. Here, too, I was subject to the whims of the doctors treating me, as no one even informed me that I had this infection, nor could any of the doctors agree on which antibiotic I needed to combat it.
I was on a whole slew of medications and was getting weaker and weaker. My digestive system, so compromised after the surgery, couldn’t handle the strong antibiotics. Shortly after, I developed MRSA (a staph infection resistant to some treatments) from all these antibiotics.
I felt so awful. I had debilitating abdominal pain, weight loss, diarrhea, nausea, and had trouble keeping food down. Eventually, one specialist realized what was going on and prescribed the proper antibiotic intravenously. I recovered, but the entire episode left me distrustful of doctors. I began going to therapy to help me cope with the resulting PTSD.
The surgery itself hadn’t been completely successful, and I was suffering from intestinal difficulties even worse than before surgery. My bowel and my body were severely deconditioned. I tried a variety of holistic medical providers, diets, medication, therapies — anything to alleviate my suffering.
At that point, I was in touch with a Jewish agency, which had advocates and medical liaisons within the hospital. The formation of this group has been transforming the health and care of patients by helping them navigate the healthcare system.
They recommended I go for a second opinion and highly recommended a top colorectal surgeon, one of the best in the province. I already knew this doctor since he’d performed a minor procedure on me, and I was moved by his patience, kindness, and exceptional bedside manner. I asked to be transferred to his care — the best decision I ever made. This doctor was a real mensch. Although a non-Jew, he was very in tune with the Jewish communities’ needs, providing care in a sensitive manner.
The doctor used to ask me questions on Jewish life like, “What exactly is cholent? Because it tastes good and has good fiber!” I felt much more confident in him than I had with my previous surgeon.
We tried different treatment approaches, but nothing helped my levels of discomfort, and four years after my first surgery, we agreed to plan elective surgery to hopefully resolve my original intestinal problem.
My sibling had just gotten engaged, and I pushed to have the surgery within the next two months so I could make it to the wedding in the US. Looking back, the urgency and timeline saved me from a situation that could have ended very badly.
At that point, I was also experiencing an onset of issues with my bladder. I was constantly in need of the bathroom, using it more than twenty times a day and frequently waking up at night. Certain positions, like bending over, caused me intense pressure and pain localized on my right side. It felt like a cluster of grapes was stuck inside me and I was feeling very bloated. Furthermore, I experienced a great deal of pain each month. I tried medication, but my symptoms worsened.
My doctor suggested I consult with a urogynecologist, who specializes in treating both bladder and female gynecological issues. I repeatedly asked that she send me for an ultrasound to see what was causing these new symptoms, but she dismissed my suggestion and told me I had an overactive bladder and that most of my problem was psychological. She hypothesized that my anxiety was creating a vicious cycle between my mind and body. She said that the more I used the bathroom, the more I would feel the need to use the bathroom.
I accepted her diagnosis and somewhat believed her, although my intuition told me that something just wasn’t right.
I was approaching the date for my intestinal surgery, and the one main concern on my mind wasn’t the impending surgery or the accompanying pain, but how I would manage to use the bathroom shortly after surgery. The whole topic was taking over my life.
I went into the operation, which was supposed to take an hour and a half. When I woke up from the anesthesia, my doctor looked at me with a compassionate face and said, “I must apologize to you for all you went through. I don’t know how you managed all this for so long. We found and successfully removed a cyst the size of an orange.”
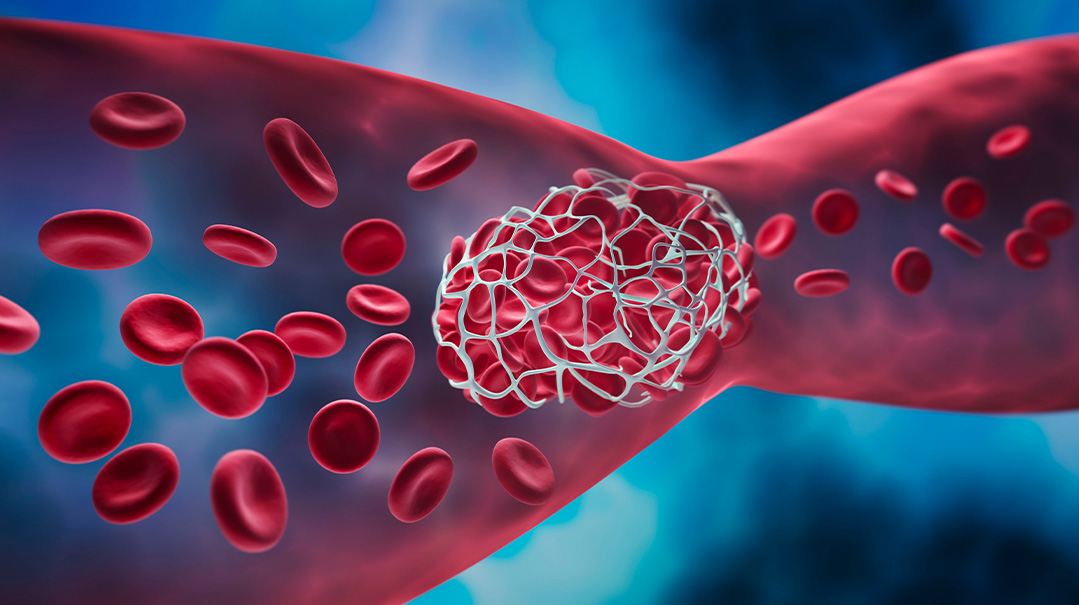
I was so groggy. I had no idea what he was talking about. But as the anesthesia wore off, I realized that the surgery had turned into a much bigger surgery than planned. As my colorectal surgeon began the surgery, he moved my intestines, and discovered a cyst adhered to my right ovary, wedging itself between my bladder and intestines. The cyst was six centimeters in diameter, an enormous size for its location. It was very solid, clearly not able to dissolve on its own.
Realizing the danger of this large growth, a gynecologist joined the surgery team and performed an ovarian cystectomy, removing the cyst. Pathology diagnosed it as a mucinous cystadenoma, thankfully a benign cystadenoma.
However, the doctors were shaken at its size and my doctor told me that if they hadn’t discovered it then, it could have ruptured within days or a couple of weeks max, causing significant damage to my nearby organs, including my intestines and bladder, possibly even destroying the ovary. This elective surgery had saved me from all that.
Immediately after the surgery, I experienced relief from the intense bladder urgency and pelvic pain, and my gastrointestinal issues were improving. The weight of the cyst pressing on so many internal organs had certainly contributed to many of my symptoms.
That was several years ago. Since then, I’ve become very vigilant in paying attention to my body and my overall health. At the beginning of the pandemic, I began experiencing discomfort and similar symptoms in the same areas as before. Although most medical appointments were cancelled due to Covid, I managed to see a specialist and have an MRI, where they discovered several small cystadenomas growing on both ovaries. Thankfully, these were able to be drastically reduced to micro size with medication.
It was another lesson to be my own advocate and to be proactive about my health. Although my cysts aren’t cancerous, such growths can be life-threatening if not caught in time.
Through this experience, I learned to be my own health advocate, and I learned some important rules for life. If something hurts, or doesn’t feel right, don’t give in and listen to a doctor who dismisses those concerns. It pays to always seek a second opinion. You know your body best, and sometimes you can be the best diagnostician of when something is really a concern. It may not feel comfortable to be demanding or assertive, but it’s your body, your health, your life, and at the end of the day, that’s what truly matters.
An ovarian cyst is a sac filled with fluid on an ovary or inside it. While many women have ovarian cysts, most aren’t dangerous.
Symptoms
- Most cysts don’t cause any symptoms. However, a very large cyst can cause:
- Pelvic pain
- A feeling of fullness in the stomach area
- Bloating
More serious symptoms are:
- Sudden severe pain in the pelvic or stomach area
- Fever
- Vomiting
- Shock
- Cold, clammy skin
- Quickened breathing
- Light-headedness
Causes
Most ovarian cysts develop as a result of a woman’s monthly cycle. Ovaries normally grow follicles, similar to small cysts, every month. Sometimes, a normal monthly follicle keeps growing, and this becomes what’s known as a functional cyst.
Contributing Factors
The risks of having an ovarian cyst are raised by:
Hormonal problems
Pregnancy
Endometriosis
Severe pelvic infection
Previous ovarian cyst
Possible Complications
Ovarian torsion: Dermoid cysts and cystadenomas can become large, even forcing the ovary to move and twist, which is extremely painful and can slow or stop blood supply to the ovary.
Rupture: A large cyst carries the risk of rupturing, causing internal bleeding and intense pain.
Information from The Mayo Clinic
(Originally featured in Family First, Issue 788)
Oops! We could not locate your form.