Restless
| August 26, 2025Our son just couldn’t seem to succeed in school. And the culprit was something we’d never expected

The afternoons when my wife was in graduate school were the hardest part of the day.
I was alone with baby Rephael for a few hours, and before long, he’d be frantic with hunger. But no matter what I did, I couldn’t coax him to take his bottle. He nursed perfectly, yet each afternoon when she went to school, he chose to starve rather than accept the rubber tip I tried to slip past his clenched lips. I was frustrated and confused, my arms aching from rocking my miserable infant son
Other than that, Rephael was an adorable baby who grew quickly and hit all his milestones on schedule. He had some minor speech issues, like saying “school” without the “s,” which we considered cute (although we did start speech therapy), but otherwise he developed well. As a toddler, he was energetic and endlessly curious, his boundless energy only escalating as he got older. He was a lightning streak, a mercurial, impulsive child utterly determined to test the limits of gravity at every turn.
By yeshivah ketanah, Rephael was the kid teachers worried about when they saw his name on the roster. He couldn’t sit still, couldn’t focus, and was constantly disrupting the class. He wasn’t defiant or malicious — he simply seemed physically incapable of controlling his energy or attention.
“He needs to be evaluated for ADHD,” became the mantra at every PTA meeting. The school pushed us toward expensive neuropsychological testing, costing around $4,000, which concluded that Rephael was hyperactive and inattentive, needing medication and behavioral therapy. We were concerned about the potential addictive nature of medication, so we spent an enormous amount of time and money on other therapies. In the end, we relented and gave him an extremely small dose of ADHD medication as well.
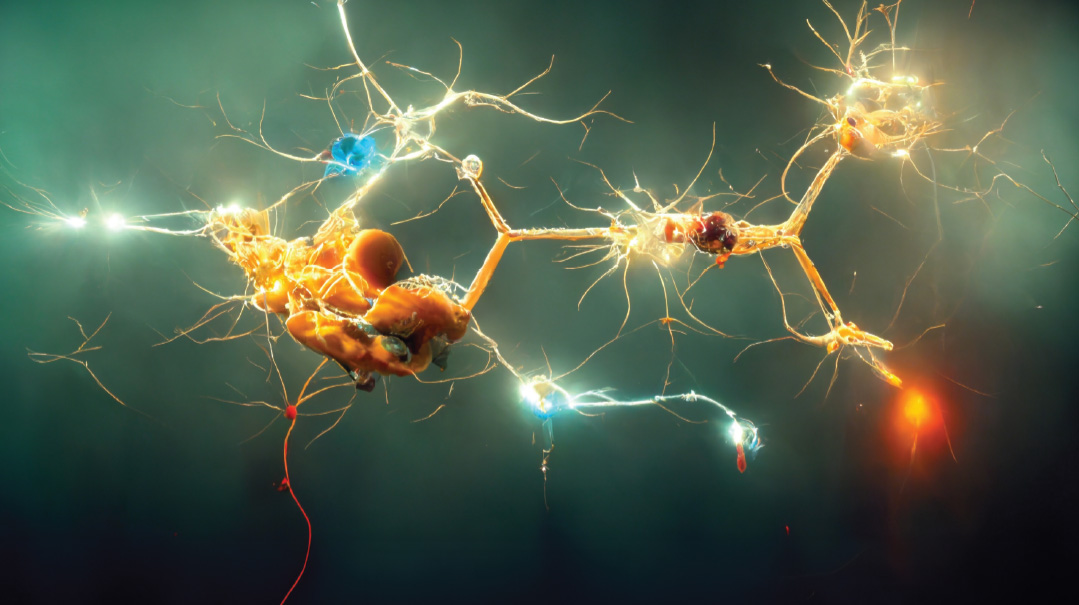
It was painful to watch my son labeled a “problem child.” His skills failed to develop because he was completely inattentive. The negative feedback loop was crushing — the more he struggled to sit still and pay attention, the more negative attention he received, and the worse things became.
Then, in middle school, something changed. The hyperactivity that had defined his early years faded, replaced by a different issue. We still got calls from school, but now the complaints were the opposite: Rephael was mentally checked out and unable to engage with his lessons. At home, he was a lot less active, preferring to sit around the house more and more. In the morning, he struggled to make the school bus, but we attributed that to the demands of middle school minyan and the teenage sleep cycle. Sometimes Rephael wanted to get up — he had friends and activities he enjoyed — but he simply couldn’t.
His mild speech difficulties continued. He struggled to get certain words out. We had him evaluated, but the speech therapist laughed us out of the room, saying that it wasn’t stuttering. However, another, more well-trained speech therapist did identify some issues and helped him.
Worried and desperate, we finally visited a sleep specialist, who recommended a simple study. Rephael wore a small device on his finger overnight to monitor his breathing patterns. No hospital stay, no bulky machines — just a straightforward at-home test that promised answers.
When the results came back, we were stunned. His Apnea-Hypopnea Index (AHI) was around 10, which meant that his breathing stopped or was severely restricted about ten times every hour. For children, a normal AHI is 0 to 1 per hour; over 5 is classified as moderate sleep apnea. My 16-year-old son was suffocating in his sleep, running on empty as his body fought for oxygen, jolting his brain awake again and again. We’d missed it completely. Tall and well-built, he didn’t fit the usual image of a child with sleep problems. And wasn’t that connected to big tonsils? Rephael’s tonsils were actually on the small side.
“Pediatric sleep apnea means there’s an obstruction in your son’s airway. In his case, it’s not the tonsils, but something is clearly stopping him from breathing. And every time his breathing stops, his brain has to partially wake up and restart the process. It’s like being winded ten times an hour, all night long. His body never gets true restorative sleep,” the sleep doctor explained.
We learned that sleep apnea in kids isn’t just an “oh, he snores” issue — it’s serious. A growing brain deprived of oxygen can’t develop properly. And we found out that pediatric sleep apnea frequently displays itself as hyperactivity before puberty and switches to sluggishness afterward — exactly mirroring how Raphael’s behavior changed in middle school. Even adults who can’t breathe at night are at risk of strokes, heart attacks, and other medical issues.
“We need to treat this immediately,” the doctor said as we sat in his office, dazed and overwhelmed.
Suddenly, everything made sense. Rephael’s elementary school hyperactivity wasn’t ADHD — it was his body running on adrenaline to cope with exhaustion. His attention problems weren’t psychological, but caused by a chronically sleep-deprived brain. His inability to wake up wasn’t teenage laziness — he had never experienced a restful night’s sleep. He didn’t struggle with learning, but with an overtired mind. While we chased psychological diagnoses, learning centers and ADHD meds, my son had been silently struggling to breathe.
The first-line treatment for sleep apnea is a CPAP machine, a device that forces air through blocked airways. It’s effective, but it can be uncomfortable, especially for teens. Rephael tried multiple masks and styles, but couldn’t tolerate his CPAP. The machine was noisy, the mask claustrophobic, and for someone sensitive to sleep disruptions, adding more stimuli was counterproductive. After a few failed nights, we had to explore alternatives to the “gold standard” treatment.
We had been working with speech therapists for Rephael’s persistent word retrieval issues, but progress was slow. Then one therapist made an observation that changed everything: “Has anyone checked if your son has a tongue-tie?”
I’d heard of tongue-tie — wasn’t that something babies had that could affect nursing? — but had no idea it could impact teenagers. The therapist explained that a restrictive tongue-tie could affect speech, swallowing, and even breathing during sleep.
We found a specialist who could release the tight tissue in a quick, five-minute procedure. The real work was weeks of exercise before and after surgery to strengthen Rephael’s tongue muscles and teach him proper tongue posture.
The results were dramatic. Within weeks of the surgery, his AHI dropped from 10 to 5, then stabilized at around 3 to 4. It wasn’t perfect, but a massive improvement. No longer was he waking up gasping for air every ten minutes.
We also worked with a specialized orthodontist who crafted a custom retainer to position his jaw and keep his airways open during sleep. Combined with nasal strips to address his deviated septum, we had a three-pronged attack on Rephael’s chronic sleeplessness, and it worked.
The changes weren’t immediate. After years of deprivation, his brain needed time to heal. But gradually, glimpses of the child Rephael could have been began to emerge.
My wife noticed it first: He looked healthier, less worn down by chronic fatigue. His grades improved. He started succeeding and participating in class in ways we’d never seen.
One frustrating part of this journey remains — navigating insurance coverage. The diagnostic sleep study was covered, and a CPAP machine would have been, but most of the treatments that actually helped Rephael were not. The tongue-tie procedure was covered by dental insurance, but tongue exercises and the nasal strips were not. Insurers only pay for “scientifically proven” treatments, but pediatric sleep apnea often requires a holistic approach that addresses multiple factors, not just one fix. For example, to help Rephael’s sleep apnea, we needed an impressive lineup of medical personnel — a sleep doctor, orthodontist, ENT, tongue specialist, and tongue therapist.
Still, no medical cost compares to the emotional toll. Knowing my son struggled through elementary and middle school, mislabeled as a behavioral problem when he was battling a serious medical condition, hurts tremendously. I keep thinking how different his childhood could have been if we’d caught this earlier. If I’d known better, I would have realized that his refusal to take a bottle and his speech were clues (the tongue therapist said the behavior is common in infants with tongue-tie). I would have realized his hyper behavior was extreme. But we didn’t know. And none of Rephael’s pediatricians or even his early intervention speech therapist identified his tongue-tie or connected his hyperactivity to potential sleep issues.
Rephael’s sleep doctor said it could take a full year of treatment to see a more complete recovery, but we witnessed encouraging signs within a few months. Today, as I watch Rephael start to believe in himself again, I’m grateful we finally found the right path. At the same time, I can’t help but mourn the years we lost, the negative self-image he developed, and the academic foundation damaged while we all looked the wrong way.
Every child deserves a chance to reach their full potential — and sometimes, that starts with something as simple as a good night’s sleep.
(Originally featured in Family First, Issue 958)
Oops! We could not locate your form.