Paging Dr. Robot

Experience a Remarkable Surgical Adventure

Photos: by Tari Pensak and GBMC
Have you ever wondered what it would be like to step into an operating room and become a surgeon? The thought of being able to truly help sick and injured people get better was always something I dreamed of. How would it feel to be right there, making a difference in someone’s life?
Well, guess what? I had the incredible opportunity to experience it firsthand! The Greater Baltimore Medical Center (GBMC) in Baltimore, Maryland, hosted a “Robot-Assisted Surgery Open House”, surgery done with the help of a robot! I’m inviting you to come along on this exciting journey as I got the chance to try my hand at it.
Meet Dr. Robot
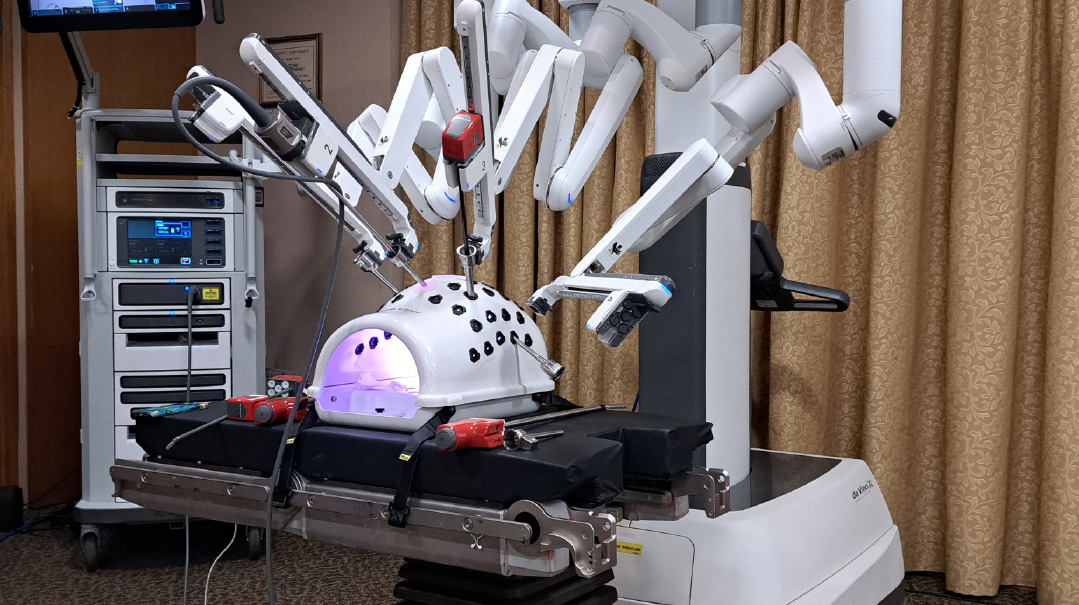
I had no idea what to expect before I got to GBMC. What is robot-assisted surgery anyway?! Are robots taking over the job of doctors who specialize in operating? Well, not quite! It turns out that a real surgeon, Dr. Emily Watters, was going to show us how she sits at something called a surgeon console that lets her control the robot’s arm movements while performing an actual operation. After her demonstration, she was going to give everyone at the open house a chance to try it out themselves.
The surgeon console had many different and interesting parts to it. There was a computer with finger loops, joysticks, and foot pedals that carried out your movements through to the robot’s “arms” on the nearby tower. These arms held different kinds of tiny surgical instruments that performed the surgery on the patient lying on the nearby operating room table.
After Dr. Watters showed us around, it was surgery time! I put my head into the console, which was adjusted to my height and view, and my robotic surgical assistant got the signal that the “operation” was ready to begin on a fake “tummy.” Inside my patient, instead of real organs, like a spleen, liver, and heart, there were different colored spikes that looked like small mountains. My job, as the “surgeon,” was to place each of the rings precisely onto the spikes without touching them. I felt like I was playing a ring toss game at Chuck E. Cheese, rather than performing an actual operation!
I placed my two thumbs and middle fingers into the two plastic loops inside the console to take control of the robot’s surgical instruments. Viewing the colorful spikes that took the place of the real organs in 3D vision was helpful; they were magnified to ten times their actual size. As instructed, I rolled my wrists around, up, and down, and forward and backward to grab the tiny colorful rubber bands. This was no easy feat! I was relieved the patient was a dummy — this operation wasn’t as easy as it looked!
When I was told that it takes months of training for the surgeons to learn how to use the robot with all its instruments, I didn’t feel as bad knowing that I didn’t get even a single ring on a spike.
Robot Surgeons in Action
I soon learned that this open house was not for the faint of heart! To make the surgeon experience feel real, a colorful video of an actual operation performed by Dr. Watters was shown throughout the open house. I was able to see the organs inside the body of an actual patient she had operated on up close — the spleen, the edge of the liver, and the heart pumping away behind the diaphragm.
What made the operation really interesting was the fact that you didn’t see Dr. Watters’ hands performing the surgery, nor did you see the patient’s body lying on the operating room table. You only saw the long thin metal wire instruments with various mini tools attached at their tips, protruding from the arms of the robot. The tools grasped, dissected, suctioned, stapled, and stitched the patient’s organs; all controlled by Dr. Watters while she sat at the nearby surgeon console viewing the organs in 3D. Her hand movements at the console were happening in real time — bending and rotating the instruments while performing the procedure. The instrument size was so miniature that she was able to operate through a couple of small tummy incisions.
What happens during a robotic operation?
First, the surgeon makes one or more small incisions. Through these incisions, the surgeon places ports (thin tubes). The robot is attached to these ports and instruments are then placed through them.
A long thin camera called an endoscope is placed through one of the ports. The camera lets the surgeon see sharp images in 3D during the surgery.
The surgical instruments are placed through the other ports, which let the surgeon do the operation.
The surgeon controls the arm of the robot while sitting at a console a few feet away from the patient lying on the operating room table.
An assistant stays next to the patient lying on the table to help the surgeon by changing the instruments when needed.
Some pros and cons of robotic surgery
Surgery performed with the help of the robot can be done by making only four or five small incisions, so there are smaller scars.
There is less pain and discomfort during recovery.
There is a faster recovery time and return to normal activities.
There is reduced blood loss.
There is less risk of infection.
The robotic arm’s movements are more exact than a person’s hand and their range of motion is greater.
The robotic arms rotate instruments in tight spaces in ways that aren’t otherwise possible for a surgeon.
The surgeon can better see what is going on inside the patient’s body thanks to the console’s sophisticated camera and 3D imaging.
Cons
Robot-assisted surgery is only available in hospitals and health care centers that can afford the da Vinci Xi surgical system and have specially trained surgeons.
The surgeon may need to change over to doing the operation the old-fashioned way with an open procedure with larger incisions if there are complications, for example, scar tissue from previous surgeries that makes it difficult for the robot to complete the procedure.
The robot can stop working, but that's rare.
The Magic
I had the incredible opportunity to personally chat with Dr. Watters. During our conversation, I eagerly asked her about the surgery details she had done in the video. Dr. Watters was not only nice and sweet, she also made me feel completely at ease. I can’t help but imagine how wonderful it is for anyone needing surgery to have her as their doctor.
Pointing to the video, Dr. Watters rhetorically asked, “It’s a pretty scary territory, right?” I nodded. Dr. Watters explained that as a surgeon, she can see everything so much better and do a much more precise surgery with the robot’s assistance. I realize that’s why she loves working with it so much.
She explained to me that she was performing metabolic surgery, also known as bariatric surgery, in the video. “The stitches are down here near the tummy and I’m all the way up near the chest. With the help of the robot, I can look down into the patient’s tummy while sitting at the console and reach into it better with its surgical instruments that I can control. The robot also makes it a lot easier for a surgeon to sew during surgery. You are able to move your wrist 360 degrees. And, you don’t have to stand on your feet for hours!”
Every single motion Dr. Watters made during this operation at the console was translated precisely to its tiny robotic instruments. Once she put her head in the console and took control of the robotic instruments, it signaled the robot that she was ready to operate. A 3D camera allowed her to see all the organs in the patient’s tummy and direct the robot-assisted surgical instruments. Her first assistant sat at the patient’s operating room bedside and changed out the surgical instruments on the robot’s arms, as needed, according to her instructions.
“It took me two and a half hours, with the robot’s help, to do this gastric bypass surgery,” Dr. Watters told me. “I had to stitch things up and rearrange how food travels through the body and how it is metabolized. This bypass surgery is one of the few things that can cure Type 2 diabetes, just by rerouting things.”
Dr. Watters mentioned that since GBMC only has one robot, that isn't always available, she must be able to do surgery laparoscopically, as well. Laparoscopy, another cool type of surgery, uses a camera to look inside the body. After putting the patient to sleep with anesthesia, so he or she can’t feel the surgery, the surgeon makes a tiny cut on the patient’s tummy. Then a really thin tube with a teeny camera attached to it is placed into it. The camera lets the doctor see what’s making the person sick so he or she can fix things more easily. With only a tiny cut made, the patient can heal faster and go home from the hospital sooner — just as they can with robot-assisted surgery.
Before I finish my stint as a surgeon, Dr. Watters tells me, “In my specialty — bariatrics, which more simply is weight-loss surgery — because I have to go through a lot of body fat during the operation, there is a really high risk of the patient getting an infection or of complications from the wound. It is easier and quicker to do it with a robot and better for the patient. Doing surgery with the help of a robot is like The Magic School Bus. You are literally inside the body and are able to see everything!”
Wow, what an incredible experience! Besides for getting a fascinating look at the marvelous human body, I can’t help but feel amazed by the world of robotic surgery. Who knows what other unbelievable things robots will be able to do in the future?
(Originally featured in Mishpacha Jr., Issue 968)
Oops! We could not locate your form.






