Three Months of Blessing

Life on a planet called the NICU. Excerpts from an informal diary, a glimpse into that world of tubes and monitors, tears and prayers

Without imposing a narrative of some kind on my experiences, I’m not sure I would have been able to function at all during this time.
From the week before our son Yehoshua Berach (Shuey) a”h was born until the day three and a half months later when he was niftar, he — and we — lived in a different universe, the cardiac NICU on the ninth floor of Columbia Children’s Hospital.
During my wife’s pregnancy with our seventh child in the summer of 2017, an initial screening indicating Down syndrome shook us greatly. We were able to get our minds around the reality and emotionally prepare for it, though, and in fact, our other children, who were becoming increasingly panicked by our hushed whispers and worried looks, were positively relieved when we told them the baby had Down syndrome — a testament to our wonderful frum community, one that treats special-needs children as valued community members rather than embarrassing secrets.
The relief was short-lived, however; further tests showed that the baby had a hole in his heart, and we were referred to a cardiac specialist at Hackensack University Medical Center, a short drive from our home in Passaic. The advanced ultrasound showed a heart defect called Tetralogy of Fallot (TOF), but the specialist assured us that the surgery to repair it could wait until the baby was a few months old. Once again, we were shaken by the news, and it took us some time to come to grips with this added complication.
We were advised to switch to Columbia Presbyterian Children’s Hospital, a world leader in neonatal heart surgery. Meeting with the team at Columbia was reassuring, as they walked us through the details of what we could expect, until and after the baby was born.
There were more surprises, as both the fetus and my wife developed a fluid accumulation that signaled significant trouble — usually some form of heart failure in the baby. But both she and the baby remained stable until 34 weeks, when distress set in. The baby was born after nightfall the second night of Chanukah, and then we began our life-altering journey into the NICU.
Precisely because of the roller-coaster nature of this journey, and the difficulty in processing cognitively (let alone emotionally) what was happening at any given point, after a couple of weeks in the hospital I started to write down what was happening around me. This wasn’t exactly a chronological diary, but more of an exercise in observation; it helped keep me grounded, it helped me make sense of what was going on around me, and it helped me deal with the whirlwind of emotions without falling apart. Without imposing a narrative of some kind on my experiences, I’m not sure I would have been able to function at all during this time.
Every few days, I would add to this document, filling in pieces here and there, tacking on anecdotes about people I met, adding information about one or another of the doctors, or noting the struggles of other parents that we came to know and befriend. Thus, these words are not so much a diary as an exercise in personal therapy, for the purpose of keeping me sane throughout this profoundly difficult time.
All in a Day
W
hen we first came to the hospital, Shuey was not yet born, so the experience for me of being in the room on the side couch wasn’t much different from our six previous births — but all that quickly changed. I’m not going to give a play-by-play of what every minute of every day was like once Shuey came into the world, but I’d like to set a common scene from a random few minutes of one day, where little slices of humanity weave their way around us, marking the hours and days in this new universe.
There are many frum families in this NICU. Parents with kids in different units float through the chesed room at Columbia — one is here for a checkup, another for surgery, and yet another with cancer. Parents meet periodically and check in on their fellow children’s status, since the nurses aren’t allowed to divulge information about other patients, even as we’re all praying for each other.
One day I went to eat lunch in the chesed room, where I met a Skverer chassid. He was eating while looking at a sefer, and began to schmooze with me in a mix of Yiddish and English, taking a great interest in the details of my baby’s situation, and telling me that the Skverer Rebbe had told him to name his preemie child before the bris as I did — although he wondered whether the name Berach, our son’s name, was a real name and not just a nickname for someone named Baruch. When I informed him that my zeide was named Berach and had a brother named Baruch, he gave in.
While talking to him in what’s left of my Yiddish, a mother came in with a rambunctious nine-year-old girl. I discovered she was from Chicago, as I am, and came in once a year for a checkup on this daughter — although she didn’t say for what. Turned out they lived in our old neighborhood.
As I was navigating this three-way conversation between her and the chassid, the most well-coifed chassidishe couple came in with a child; they were so stylish and photogenic you would think they were in an ad for a Thirteenth Avenue clothing store. He was surprised that it could take me an hour from Passaic to get over the bridge, but then again, he commuted in the other direction — from Williamsburg to some town near Wayne.
These typical short-lived encounters happened all day, and had I not written them down immediately, they would mostly be forgotten. Life in the hospital is like that. It blurs together until all recognition of independent events and people are smushed into a gummy connective mass linking discrete events — the day of the surgery, the day the baby was born, the crisis on Shabbos when the baby had gone into septic shock but honestly we weren’t really sure what happened, but we were glad it was over.
People are there because a loved one is having surgery, a parent is dying, a child is terminal, or because someone is giving birth, or being closely monitored in order to give birth safely. Everyone is the same because everyone is yanked out of the normal push-and-pull of life and thrown into suspended animation — life can’t continue normally because in the hospital it is the existence of life itself that is in question.
Since my wife was first brought into the hospital before birth, I haven’t had a single “normal” Shabbos. During the week, we’ve mostly been eating food that others have made for us, doing the bare minimum of work to get by, pushing off appointments for non-essential things since there’s no guarantee we’ll even make it to them. Having a few spare minutes to change the lightbulbs feels like a major victory.
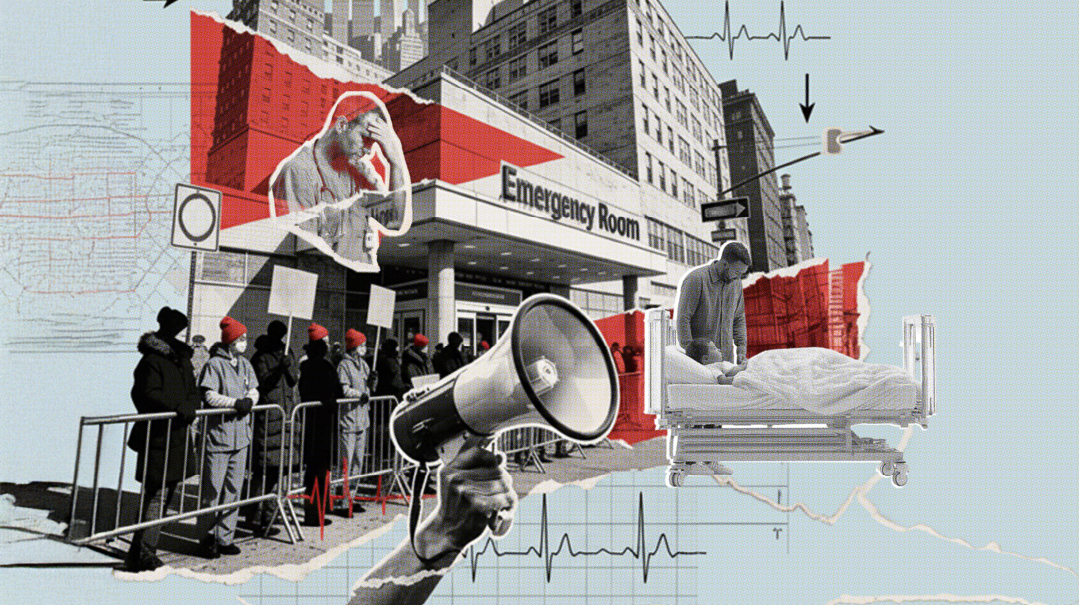
Every day, one of us sits in the hospital all day as time moves both extremely fast and slow. The day zooms by, yet it feels like you’ve been there for ages. Something is always happening, and you become a slave to the numbers — the vital signs, learning to interpret sats and maps and art lines, and the quirks of the bubbler, the vent, or the nitric. Rounds and nurses, and emergencies next door, data by the bushel all feeding into remarkable systems for processing the numbers and turning them into even better numbers, and the machines, little sci-fi tricorders that give instant data on the metabolic makeup of blood, iPhones that are also scanners that process meds and drips and pumps, while letting everyone text important info, call the doctor, call the fellow, or call the charge nurse for coverage. Giant machines come lumbering in, like beasts of burden wheeled by their handlers, to X-ray, echo, and ultrasound, probe, and prod, and slice, and dice, while you look on numbly and try not to get in their way.
The hospital staff is in this time capsule as well — 12-hour shifts through the day, through the night, a doctor on rounds in the morning, on call at night, parents coming and going at odd hours. The young mother next door sometimes shows up at 2 a.m. to stay with her very sick baby. And the parents and families who live in and out of the hospital all know this — they know they are living outside of time, in a little life raft. Their children or parents may be clinging to life, but they are in the life raft with them and though they’re not hooked up to machines, they are just as stuck; they can’t move forward with life, either.
Heroes of the Ward
T
he doctors, nurses, technicians, and other members of the hospital ecosystem are no less than heroes in every sense of the word. To observe medical rounds in a cardiac NICU is to watch the pinnacle of human achievement, and yet to realize how little we still know. The attending neonatologist, the attending cardiologist, the charge nurse, the nurse practitioner, the baby’s nurse, the nutritionist, and other people who I haven’t yet identified, all gather in a circle and the rituals begin. They review the baby’s entire history — “Baby Krakowski, now 39 days, history of Tetralogy of Fallot, Chylous Ascites, etc. etc.” — describe what’s been happening lately, and what needs to be done going forward. They take turns, as the attending doctors ask their fellows what they would do, probing them and teaching them while still trying to figure out what’s going on and what the best course is. They are all trying to figure out how to proceed, sometimes differing sharply depending on their expertise.
“Why don’t we check his levels at Q12?” asks the fellow. “Well, what would you do different if you checked it then?” the attending cardiologist responds. When she thinks about it for a minute, he elaborates, “If the levels are x then you can’t do anything because you have to check p, z, and q, which won’t be available for 24 hours anyway, and if the levels are y, you won’t know anything because of r, j, and x. So better wait 24 hours and get a better trend line so you can see if there’s a real difference.”
I actually made that scenario up, but it reflects the tenor of the conversations. There’s so much that they don’t know, even as they operate at such a high level, debating, discussing, helping, and teaching each other — yet at end of the day they walk away stumped more often than not, saying we’re going to try x and see if it works. They majestically balance hundreds of different factors, thinking through the implications of one medicine on the vascular system if the fluid buildup is from cause x, as opposed to the completely different impact if it’s from cause y, while working through dozens of different outcomes with one another to chart the best path forward. And yet. They still don’t know even a fraction of the complexity of the human body. They can stick a piece of Gortex into a tiny hole in the heart, but they still can’t tell you why the baby can’t tolerate formula.
They listen to, and respect, parents in the NICU. If you say, “I’ve seen my kid over the last few weeks and something is different now” they don’t ignore you, but they listen and look and factor that into the discussion. The doctors at rounds discuss whether upping his calories could have prompted his negative reaction, but they believe me when I tell them that problems were occurring from the beginning of feeds.
One Friday the attending neonatal doctor, Dr. Vargas, had been on rounds all day and was also on call that night, but over the course of the day the baby seemed to start breathing faster and faster and I was worried. She sat with me and assured me that they would watch him closely and check with an X-ray for fluid in his lungs if it kept up. Shortly after I left that night his blood pressure started dropping while his X-ray was clear, and they moved from watching to working, as tests were done, antibiotics were started, echoes and ultrasounds were taken, a bolus of bicarb, another bolus, two different blood pressure meds one after the other.
Dr. Vargas stayed with him all night after having been on the floor all day, and even after her handoff to the next attending doctor, another superhero named Dr. Goldstrom, she didn’t leave until mid-morning when he was somewhat more stable. She also didn’t leave before she sat with me, bleary eyed and cross-legged, and went through everything they knew and didn’t know about what was going on. They know they are at the peak of the profession and they know life and death is on the line, and they don’t have to pretend to patients that they are omniscient. What they are is good enough.
In Its Own Bubble
T
he NICU is a society, an ecosystem unto itself. There are the nurses, the doctors of different stripes, and then of course others who make their way through the little world of the NICU. Aside from the various technicians bringing their giant lumbering beasts, there are also obsessive cleaners, a handful of people who wipe and sweep and spray every surface over and over, making sure no disease infiltrates. After each room is cleaned, the mop head is thrown out and a new one attached.
Other hospital employees wander around periodically swabbing surfaces to check for the presence of disease, making sure not to leave any surface unchecked. Researchers of differing persuasions flit about, enrolling you in one or another study; the genetics team wants to sequence yours and your wife’s whole genome (along with the baby’s, of course) to find out the mechanism for certain sorts of congenital defects, some other team collects embryonic fluid to investigate lymph disorders, and the psych team wants to know how stressed you are.
The truth is that nurses and doctors live in two different fiefdoms. The nurses are like those dedicated municipal government workers doing all the grunt work day in and day out. They deal with everything from cutting the feeding tubes to the right length to changing diapers and weighing them, inserting IVs and arterial lines, checking saturation rates, bagging the babies when their blood oxygen drops, dealing with anxious parents, working out the optimal way to get enough lines into a baby to measure all that needs to be measured while also getting enough of the meds and fluids in. The nurses also see the babies all day long, learning enough about them to know their quirks — when they are fussy, how they respond to meds, what certain responses indicate medically, and so forth.
The doctors, and to a lesser extent, the nurse practitioners, might be all-knowing, but all their data comes from the nurses. What the nurses tell them or don’t, what they notice or don’t, becomes the basis for most doctor decision-making. Of course there are exams, and labs, and X-rays, but for the most part, there are nurses. And though the doctors rule, they can only direct the nurses in a very general way, at the level of policy, because they don’t really have much say over the day-to-day operations. In the end it’s the nurses who decide how their little kingdom works.
Then there are respiratory therapists, whose appearances are triggered by a doctor saying the baby needs setting x on the ventilator, the nurses calling the therapist and the therapist coming in peering at a sheet, at the monitor, and then briefly adjusting a dial, clucking gently while noting things down and walking away. There are physical therapists and occupational therapists who come in and move the baby’s limbs around in various ways, cooing and murmuring about muscle tone. People from the machine shop come with warmers and incubators and brand-new pumps, and pharmacy people bring drips and meds that need to be used before they expire. Nurse management officials come by to admonish the nurses to take their breaks, hospital PR staffers cruise the hallway looking for a good story to feature, and highly trained maintenance guys test the alarms and check the A/C settings, looking a bit out of place in their work clothes and tattoos.
And within this ecosystem, the parents of the babies wander through, but our role isn’t clear — do we belong here, or are we an invasive species? Doctors and nurses register our presence, and acknowledge our right to be there, although we’re more like background scenery unless we deliberately get their attention (at which point some of them might politely do what they must to placate us until we quiet down again, much like one of the pumps acting up for a few moments). There are some uncomfortable chairs for parents to sit in and even lie down, but they clearly don’t expect the parents to do so — there’s barely enough room to open the chair into a bed; the lights are on 24 hours a day and the nurses are busy all day and all night. Sometimes we get the feeling that they’re thinking, “We know you have a right to be here but you’re not very important, and honestly wouldn’t it be easier for everyone if you went home and let us do our jobs?”
They don’t actually ever say that, and they do listen to us and value our input when we have things to say about our babies’ care, but the structure of the NICU makes saying it unnecessary; it’s built to push us to the margins.
When talking to each other, and to parents, NICU personnel develop a language of euphemisms: “He’s not so happy now” doesn’t have anything to do with his emotional state, but rather his wellbeing — his pain, his vitals, or his need for external support. Similarly, “it was an exciting day” is not a good thing, but a description of a day when things went wrong — a baby coded on the floor, multiple babies came back from the OR and needed close care. They also use acronyms for everything — they don’t just say he needs breast milk, rather “he’s on EBM” (expressed breast milk); he doesn’t have Necrotizing Enterocolitis, but NEC. They pepper this shorthand back and forth to each other as they navigate the unit, hoarding supplies that are running low, such as tubing, needles and lines, special pillows and seats, “mustaches” and tape of various kinds (to hold the CPAP on), and glycerin and other meds to have at the ready.
There is an interesting dynamic among the nurses. They hang out in cliques like any social group, and sometimes you hear them gossiping in the hallways, but for the most part they are extremely sincere and devoted, and many of them come from religious backgrounds and are people of strong faith.
Sometime it seems like arts and crafts time — cutting and pasting or using safety pins and rubber bands to find ingenious ways to keep the baby’s tubes from coming out, to hold his hand down so his line doesn’t get ruined, to keep his hat on his head or his oxygen flowing properly. They make mini beds out of blankets and tape, and use scissors to cut pacifiers so that they don’t interfere with the CPAP in the baby’s nose. They use and dispose of truly gargantuan amounts of supplies, new gloves, new wipes, new everything, every time they get up from their desks.
They also know that they have to manage the parents as much as the babies, and some are better than others. I’ve been admonished more than once to stop worrying about the monitor, yet at the same time many nurses recognize that this is natural, and that it’s hard to be a parent in this situation. One evening I had a long conversation with Nurse Paulina about this very phenomenon. She told me that her attitude shifted completely when her brother was admitted for a serious surgery. Staying with him, she lost all of her professional cool and spent the entire time glued to his stats in terror.
Nurse Katie, who gently chided me about my concern, acknowledged that parents are the most observant of all the people here, and that it’s their job to listen to our concerns, since we are most likely to know what’s going on. When I mentioned that some nurses seem to get irritated if you point out too much, she grunted and said, “Well, they need to get over themselves.”
Days of Rest
T
he hospital on Shabbos is a world of its own, especially in Columbia where all the Jews congregate together. There is a minyan kavuah with two sifrei Torah, hot food in a warmer provided primarily by Skverer and Satmar chassidim, and also by other groups, including Chai Lifeline. Grape juice, challah, cholent, and kishke all are readily available in great quantities. The food in the kosher room is all very heavy and heimish, but not bad for the most part, and sometimes really good.
The people who run this chesed are amazing; they take care of every person who comes through looking for kosher meals. There are apartments with beds nearby (courtesy of the chassidim and the local kehillah), seforim, toys, and videos. They call to check up on you, and they know what your story is. Nobody asks for anything from you — they just give with a full heart, and keep on giving. Whether you’re Satmar, Lubavitch, modern, yeshivish, or Yemenite Israeli, everyone unites and takes care of one another. Nobody cares about anything else; they’re b’achdus in a way that’s remarkable.
Because of the different reality we’ve all been thrown into, all the petty squabbles of reality have no purchase here. The first Shabbos I was surprised when we didn’t have a minyan for Maariv and ten minutes after tzeis hakochavim three chassidim walked in looking to daven Minchah. Some weeks later I was even more shocked to see a chassid on his phone as we davened Kabbalas Shabbos well past shkiah — but when I spoke to him later I learned that his phone conversation was a case of pikuach nefesh. He was a caseworker for Refuah, an organization that gives medical referrals to frum people, and had come into the hospital with a friend whose 18-month-old daughter had been acting strange. As soon as they CT-scanned her they rushed her to surgery to shunt fluid off the brain as they prepared for a larger surgery immediately afterward to remove a giant tumor. This askan was on the phone with an expert at Cornell to determine whether the approach the doctors at Columbia wanted to take regarding the surgery was really the best approach.
During davening people with no apparent care in the world sit next to those for whom the world is clearly too much, and no one begrudges anyone else their suffering as too small. There’s even one man who feels guilty that he is not as bad off as many other people. He’s been here since after Succos when his wife was admitted with pregnancy complications, but nobody resents his good luck. And besides, it’s not easy living for months in the hospital even if your loved one isn’t dying. (In fact, I met him in the chesed room a while later and he was wearing three wristbands. He informed me that after the months of complications, his wife gave birth to three healthy baby girls, all breathing and eating on their own. It’s hard to describe the happiness seeing someone go through close to three months of hospital life, a major trauma at birth, and have the outcomes all looking positive: Overwhelming happiness to the point of tears, as well as a little tinge of jealousy, to be honest.)
Another father who was here the first few weeks was a complete wreck, and for good reason. He walked into Shacharis the first Shabbos I met him and exclaimed “another horrible day” telling me how his only child, a three-year-old, has been in an induced coma for the past two and a half months, and would go into cardiac arrest if woken. The child had a disease so rare that it doesn’t even have a name — it’s only defined by letters and numbers. He told me that he spends 18 hours a day every day in the hospital, and indicated that his marriage was falling apart from the strain. He had been trying to arrange a transfer to another hospital where there was a doctor who had done research on a similar rare disease and might have some insight into this one as well. I hope that’s the reason he disappeared shortly thereafter.
Which raises an emotionally complicated aspect of hospital life. None of the staff can tell you anything about other patients, so you connect to and worry deeply about them, but they disappear and you can’t even find out if it was because of death or good health. Emergencies happen across the hall and you are ushered out as they call “Code Blue,” and after they’re done working for a few hours you have no idea if that baby is even still alive, while the heroic nurses and doctors retreat, exhausted, back to their regular assignments.
Shabbos on the Ward
D
uring the week, you only have a chance to meet other frum people for short periods of time, but on Shabbos, when you are, in many respects, trapped, the hospital becomes a different sort of place where you have a chance to engage with others, hear their stories, and establish a tenuous community. My Shabbos routine in the hospital is fairly stable. I get to the hospital an hour before candle-lighting and unload my bathroom tissues, my Gemaras (Steinsaltz for the week’s daf yomi — which I do all of on Shabbos — a regular Gemara for the daf shavuah, and a small ArtScroll to check my understanding of the daf after I’ve completed it), another sefer called Lachem Yihiyeh L’Ochla by Eitam Henkin Hy”d — the young illui who was killed by terrorists together with his wife in 2015, my tallis and siddur, a sci-fi novel, my computer, wallet, keys, and a bottle of seltzer. I gather up the food left for me by the chesed organization at the receptionist’s desk (no food allowed in the unit itself) and sort and label it.
Even though the elevator to get to the kosher room on the sixth floor is just across the PICU unit from me, I am not officially allowed to walk through there, so I have to go down from the ninth floor to the lobby, walk across and go back up the sixth. This is not so bad during the week but it’s a major inconvenience on Shabbos. I head to the kosher room, put my labeled food in the warmer and my cold food, juice, and challah in a labeled bag in the fridge, and then take my toiletries, pajamas, phone, and contact lens case to the Skverer chesed house, which has separate apartments for men and women.
At the chesed house I find my bed, meet my roommates, and plug in my phone. If there is an emergency at the hospital while I sleep they will call this phone, and although I won’t answer I’ll rush over. This has happened once so far, and I hope it doesn’t happen again (it didn’t). Now roughly candle-lighting time, I rush back to the baby’s room, check in with the nurse, and then head back to the kosher room. At first I would head down before shkiah, but I have since learned that given how many chassidim populate the hospital, Minchah is never before shkiah and I can comfortably wait quite some time before heading to davening.
At this point, though, melachah is no longer allowed and life gets very interesting. The doors to the hospital have electronic eyes, the NICU unit itself is guarded by an electronic pressure plate door, the bathrooms all have electronic eye flushes, and most have electronic sinks as well. The Purell dispensers and soap dispensers are electronic (and mandatory) and hands need to be washed with soap before entering the room. There’s one elevator near my unit that runs on a Shabbos mode (though they occasionally forget to turn it on until mid-morning on Saturday) and there’s a stairwell that I can use from the ninth floor. The elevators by the kosher room also include one with a Shabbos mode, but the stairwell is electronic access only, so it doesn’t help. This means that to get to the kosher room I have to wait a very long time for multiple Shabbos elevators stopping at every floor, or use the stairs-and-elevator combination. I ask the nurses to prepare some water in a pitcher and soap in little packets for me in advance, and I follow the halachic guidebook I have for navigating the bathrooms when I need to use them. I stand by doors awkwardly waiting for others to go through them or for nurses to hit the button for me, and mostly, because of these issues, try to stay in one place.
At Minchah-Maariv Friday night there is usually a mix of different types of chassidim and a few others, and it’s usually a chassid who takes the amud, though not always. After davening, there is an inevitable discussion about moving Shacharis later than the posted eight-thirty time — nine or nine-thirty is the usual result — and people scramble for the warmer and the fridge to get their food and go back to their rooms for a meal. I am one of the only people who eats in the chesed room since I can’t bring any food to the NICU. But the upside to this is that I get to sit and talk to the other people who come in and out.
A few weeks ago, for example, I sat and talked at length to a remarkable man, a Skverer chassid who lives in Monsey and was in the hospital with a critically ill ten-month-old baby with Down syndrome. It turns out, however, that he’s the foster father of this child. In some chassidic communities, families who have babies with Down syndrome are advised to give them away to foster care. The parents of this baby wanted to keep him, but their rebbe encouraged them to give him up. This fellow sitting across from me took the baby in, he told me, not as a favor to them, but because his own youngest was five and he and his wife wanted another child in the house. He told me how late one night the birth father and one of the sisters came by to drop something off, and after closing the door he realized that the reason they came by so late was to see the baby. And so he went back out and invited them in. He told me that he invited the birth parents to come by whenever they wanted, and they did come by occasionally — although some of their other children refused to acknowledge that the child existed.
This man had a beautiful description of life with a child with Down syndrome, which spoke right to my heart. It wasn’t the usual discussion of special neshamos waiting to come down to special families, important as that idea is. Instead he told me that I would see that our baby would be a source of unparalleled joy. With a Down’s child, he explained, you don’t project any of your own expectations onto the child, and you don’t judge them for failing to be something they’re not. You just appreciate who they are without expectations — whatever they do is a source of joy, whatever they do is nachas, and it’s not measured against what you want them to do. You can simply appreciate them for who they are.
After my seudah I go back to the room and sit with the baby, learning one of my seforim and watching the baby’s numbers rise and fall. After the nighttime rounds I head back to the chesed house to sleep, which is a bit awkward at first — a bunch of strange men thrown together under circumstances beyond anyone’s control.
I still remember that Shabbos when my phone rang in the wee hours of the morning, and terrified, I ran the two blocks and climbed the stairs to the ninth floor to find the baby in a state of shock. They had waited to call me until this point because they wanted me to get some sleep and not be going crazy in the hospital. Baruch Hashem, the baby recuperated from that episode, but every time I go to sleep in the chesed house I’m in a slight panic, anxiously dreading the sound of that phone. When it doesn’t ring, I get up in the morning, go to the hospital, and get some coffee from the kosher room. I then (carrying two extra coffees) go back down the Shabbos elevator, cross the lobby and go back up the Shabbos elevator to the 9th floor (assuming they remembered to turn it on) and check in on the baby. I sit there learning until rounds, and then make my way back to the chesed room to see where they are up to in davening.
Because davening never actually starts at eight-thirty, I’m usually not drastically late as I greet the ragtag crew from the previous night with a look of recognition, checking up on how they’re all doing. Leining is always an adventure, and it’s usually a scramble to figure out who will do the least bad job. Sometimes one brave person will start after others have demurred, but when they see how bad he is they’ll change their minds.
During davening non-Jews come through the lounge where we daven, trying to access the bathroom, microwave, or soda machine. For the most part they try very hard not to interfere with prayers, and are reluctant to walk through — although it is very important to let them. This is both because it is not our private space, and because once when a very nice young woman didn’t want to disturb “the rabbis” she went into the kosher room (the door had been left open for fresh air) to microwave her treif food there. Had I not been wandering around during davening, she probably would have used the microwave. Instead I assured her she could walk through with no problem.
At some point during our stay here, I’ve been living in the hospital so long that many people on Shabbos think I’m the chaplain, since I know the code to the aron and seem to know my way around. I let people know what they can and can’t do, and what the minhag hamakom is for davening. It’s those like me, in for the long haul, who keep the minhagim going. One of those minhagim is to argue about what time to daven Shacharis, Minchah, and Maariv.
Despite the bickering over zemanim, the 20 or so people interact with one another as if it were a real kehillah. The last Shabbos I was there, I didn’t see the father of the girl who had come in with the brain tumor so I made a Mi Shebeirach for his daughter. After davening another man came up to me to thank me, saying he was the brother of the father, and that he was staying with his brother in the hospital for Shabbos, though his brother had walked to another shul that morning. I had beaten him to the Mi Shebeirach, but he was appreciative that I had thought of his niece. This is part of the natural areivus such an environment generates.
Over the course of Shabbos, I have time to talk to people and hear their stories, and tell mine as well — something that is therapeutic and calming. One week it’s a man originally from San Diego who lives in the neighborhood, who schmoozes with me about architecture in Chicago while waiting for his newborn’s breathing issues to clear up. Another week it’s a teenager with skinny jeans accompanying his father while his grandfather is admitted.
One Shabbos, my roommate in the chesed house is the fashionable chassidish fellow who had been in a week earlier. His three-year-old son was undergoing his third and final surgery to correct a heart defect, and by this point he was a mumcheh in heart issues. Later that day I met a chassidish woman who came to the chesed room looking for Kiddush. She’d just given birth to a baby with the same heart defect and was waiting for a space to open up in our unit. When I mentioned this to the chassidish fellow, he was very excited and told me that if I saw her I should tell her to stop by his child’s room to speak with his wife. In fact, moments later when I stepped into the elevator and saw her there, I told her about his offer.
The Last Chapter
A
fter all we’d been through in the past months, nothing could prepare us for the final week of our son’s life — yet that’s when we felt the care and support of the doctors and nurses most profoundly. It’s hard to write about that terrible time, but it is enough to say that within the span of one morning, our son went from being basically fine, and undergoing tests to see if he would be going home with a feeding tube or g-tube, to undergoing emergency surgery to see if his intestines could be saved. They were not able to save his intestines, which appeared to have been hit by a mysterious and poorly understood disease: necrotizing enterocolitis in its fulminant form — which is a fancy way of saying that it went through his system very fast, killing his intestines completely over a matter of hours. The shock and devastation have not worn off.
They told us late that evening that they would give him two days to see if any of the intestines were salvageable, and over those two days the support we received from our kehillah, from our extended family, from people far and wide, who we barely even knew, was beyond anything we could possibly repay. The Tehillim and the tefillos that were recited were powerful and meaningful. As we sat in shock at the baby’s bedside, other people mobilized to take care of our family’s physical and spiritual needs.
Two days later, on Shabbos morning, the doctors confirmed that there was nothing to be done, that nothing in his gut was able to be saved, and that he was going to die. At that point we had to call both our rav and a more prominent posek to find out what we should do. The next four days, until he was niftar, were the most painful ones in our lives, and I cannot write in any detail about them, because the pain is too great. What I can say is that unlike what we hear from European countries about how they treat sick babies and families, America is a medinah shel chesed, and the doctors and nurses were all completely supportive of whatever choices we made.
From the doctors’ perspective, the best thing to do would have been to say goodbye and then take him off the ventilator, which our posek said was forbidden. But when they briefly misunderstood us as saying we wanted them to work as hard as they could to add aggressive support to keep him alive as long as possible (which our posek also said was forbidden, given the fact that it was not a question of if, but when), they were completely willing to shift what they were doing and reintroduce complete affirmative care, rather than just palliative care. Ultimately, the specific instructions from the posek were so complex (don’t renew the antibiotics and don’t go higher on the ventilator settings, but don’t stop nutrition and fluids, etc.) that the head of the unit herself got on the phone with him to work through the specific rules for our son’s treatment, and they followed those rules without question.
The next four days were filled with doctors and nurses coming by and sitting with us, crying with us, and doing everything they could to give my wife and me time to hold our son and be with him. He was so fragile that three nurses needed 15 minutes of work every time he needed to be moved out of my wife’s arms, but they were more than happy to do so. They let all of our children come and see him despite the age rules, and they let us live in the room, bringing our food in as well. He was finally niftar on 5 Nissan 5778 — March 21, 2018 — during a terrible blizzard, and there were nissim v’niflaos involved in getting a levayah and burial done on that day, as the cemeteries did not want to stay open. To our shock, between one to two hundred people, with only 45 minutes of warning, showed up in the blizzard.
I will close with the brief words of hakaras hatov that I shared at the levayah, since hespedim are not said in Nissan. When, as a child, you are taken on a once-in-a-lifetime trip or experience with your parents, it’s natural to be thankful to them, and express that thanks when you leave. Life, every second of it, is a once-in-a-lifetime experience, and the amazing gift that Hashem gives us has to be acknowledged. Both my wife and I felt profound appreciation to Hashem for every moment that we had with our son, for the joy he gave us, for the meaning that he provided in life just by being.
At the same time it’s natural to feel terrible pain when leaving, to want just one more day, one more ride, one more, one more. Precisely because the gift is so wonderful, it is so unbelievably painful to say goodbye. If it weren’t such a precious and great thing, the loss wouldn’t be so excruciating. Our life over the three and a half months in the hospital was one built on the chesed of others, which allowed us to appreciate the chesed that Hashem built into the world, and the chesed that he gave us in our wonderful son, Yehoshua Berach. Life in the hospital is completely draining, full of fear, pain, and confusion. But it is also full of hope, kindness, love, and simchah, and having been in that situation, we can fully appreciate the world of chesed that Hashem created all around us.
(Originally featured in Mishpacha, Issue 733)
Oops! We could not locate your form.