Sense and Sensitivity

“What really matters is the person’s level of functioning,” Jerusalem-based occupational therapist Chava Zehava Fleischmann explains, “how is it affecting her life, what are the areas in which she feels limited, does it constrict her in any way, and how”
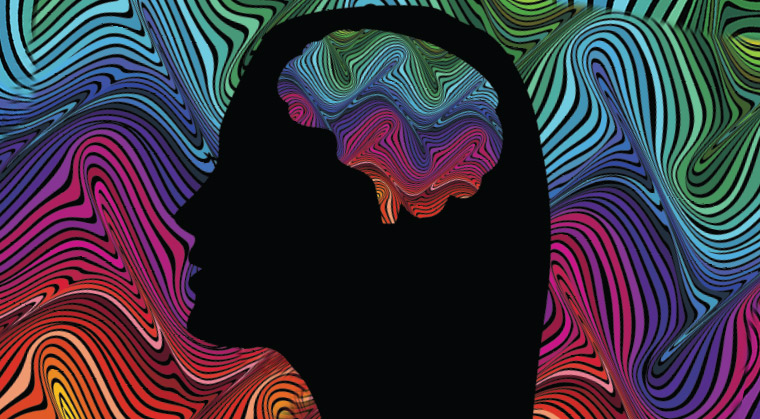
Bothered by the sound of fingernails on a blackboard? What if you also feel that way when touched from behind or unexpectedly? You’re exasperated by the volume of your kids’ music, tense up from the smells of your coworker’s lunch, and feel thrown when things get in the way of your perfectly planned weekly schedule. Anxiety, control, and overwhelm are just some of the terms that have been tossed at you, but you wonder: What if there’s another explanation?That Makes Sense
When bright lights or noisy crowds or seemingly normal smells and tastes drive you crazy — something more might be at play. The role sensory processing plays in our lives and what happens when the processing isn’t smooth
THAT MAKES SENSE
You may have always been this way, but suddenly, as an adult, it matters. It matters, because no longer are you the child whom people forgave for her quirkiness; it matters, because when you snap at your toddler who reached out to stroke your face, or when you react to your spouse’s early homecoming with frustration because you just weren’t ready for him, not yet, there’s too much going on, you know it’s stopping you from being the person you want to be. It matters so much that you start to hate yourself for being this way. You’re frustrated and so are the people around you. Nobody is able to make sense of your reactions, of your intense need for things to be a certain way — least of all yourself.
If any of that sounds familiar, you’re probably well acquainted with terms like panic, anxiety, OCD, and depression. But somewhere, something niggles; you know that can’t be the whole story. How does it sufficiently explain why you hate noise and bright lights and recoil at the slightest form of touch? You often feel dizzy, you avoid heights, and you get nauseous each time you travel — why?
Questions like these followed Rachel S. Schneider, MA, MHC, over the years, as she struggled to find an explanation that would tie together the gamut of her frustrating experiences. And then, in 2010, at age 27, she stumbled upon some interesting research and finally had her lightbulb moment: She wasn’t crazy or impatient or obsessed — she had sensory processing disorder (SPD), a neurological condition that impacts the way one processes the information that enters the nervous system through the senses.
Later, Rachel would go on to establish a website on adulthood SPD, as well as author the blog Coming to My Senses, which, she says, provides an intimate picture of SPD diagnosis and treatment in adulthood. In 2016 she published her first book, Making Sense: A Guide to Sensory Issues, in which she uses a combination of plain English, a good dose of humor, and thorough research to help people understand adulthood sensory issues and the struggles that accompany them.
ALL SYSTEMS GO… OR NOT
What is sensory processing anyway?
When a sensory stimulus entering the system — say, a bright light or a soft touch — is not adequately processed, the body cannot respond appropriately; hence the terms sensory processing disorder or sensory integration dysfunction. Stimuli can come from any of the senses — sight, hearing, taste, touch, smell, as well as from the proprioception (the body’s sense of position, orientation, and location in physical space), interoception (the internal sense that tells us what our body needs to function), and vestibular (balance) systems.
When the systems work at a healthy level, responses are either negative or positive but are appropriate given the input (snatching your finger away from a hot iron, for example, or feeling excited upon hearing music at a wedding hall), and for the most part, performance and function are optimal. When the system goes awry — in sensory lingo, lacks organization — and the brain perceives certain input as a threat, responses become disproportionate in relation to the input, and can be either physical or emotional. A common example of this, says occupational therapist Miriam Manela, founder and director of The Thrive Group, a New Jersey–based occupational therapy clinic, is responding to an innocent brush on the shoulder by reciprocating with a shove. An emotional response might be a sudden intense need to yell or cry or run away and hide.
I HAVE WHAT?
There are several categories of SPD, and then further subtypes, each describing the different ways sensory stimuli are processed and reacted to (see sidebar). But the most concerning type seems to be the sensory avoider, or the “over-responder,” because “the sensitivity associated with those who are over-responsive is usually pretty intense,” speculates Rachel in her book. It’s hard to survive, let alone thrive, when you’re constantly feeling overwhelmed, she explains.
In fact, it is this category of people that Sharon Heller, PhD, targets with her book, Too Loud Too Bright Too Fast Too Tight. “As many as 15 percent of otherwise normal adults have a nervous system that is overly sensitive to sensation,” she writes. But incidentally, nowhere does the term SPD appear in the book; “sensory defensive” is the term given instead, applying to the whole spectrum of people, from those able to “grin and bear it” to those who find even minor stimuli “unbearable.”
Like all diagnoses (if you can call it that — while gaining recognition, SPD is still not recognized by the DSM-5), SPD runs on a continuum from mild to severe, says Miriam. And some people are uncomfortable with the term altogether, contending that their experiences are not severe enough to associate with a “disorder.” They may prefer terms coined in the mid-1990s by psychologists Elaine and Arthur Aron — sensory processing sensitivity (SPS), or highly sensitive person (HSP). These individuals report heightened responses to stimuli, contributing to higher emotional reactivity and lower risk-taking behavior.
But what’s integral here is not the label or terminology, says Jerusalem-based occupational therapist Chava Zehava Fleischmann, who specializes in sensory integration and works with adults and children. “What really matters is the person’s level of functioning,” she explains, “how is it affecting her life, what are the areas in which she feels limited, does it constrict her in any way, and how.”
This approach is one that Chava Zehava also encourages her clients to take. “Who cares whether you think you have SPD or whether you’re certain that you don’t, or if you think you have anything else, for that matter? If you feel your function is compromised in any way, let’s look at that, and see how we can get you back to function.”
Interestingly, says Miriam, most of her clients do not qualify for any diagnosis, but find their way to her out of frustration that they’re not able to function comfortably in their environment.
And that, above all, is what seems to be key here. While sensory processing and function are so closely intertwined, people get carried away by the sensory processing aspect but do not pay adequate attention to what they really need to be concerned about: how much of it disrupts your life, does it rule the choices you make, and what sort of emotional upheaval are you left to contend with.
CAUSE AND EFFECT
What exactly goes wrong for people who struggle with sensory processing?
That’s what researchers have been trying to uncover for years — what causes inadequate sensory processing, and if and how it presents in the brain’s physical matter.
There are three main possibilities, but they don’t explain all cases: genetics; allergies, illness, or exposure to environmental toxins; and trauma. “Any trauma that disrupts the nervous system at any age can generate sensory defensiveness,” writes Dr. Heller. This may include prenatal or birth complications, head trauma, abuse, or post-traumatic stress disorder. The trauma need not be major, says Miriam; in fact, anything that lodges in the brain as a threat, such as persistently hearing a negative comment from a close family member, for example, can fall under the “trauma” banner.
What happens is that the nervous system stops differentiating between real or perceived threats, says Dr. Heller, which means that the body’s normal protective response is exaggerated and harmless sensations are perceived as dangerous. In self-protection, a person might leave a social event abruptly or snap at an innocent bystander, “unwittingly reacting out of proportion to the situation but in proportion to a brain that perceives danger.” The body doesn’t have time to rationalize, Dr. Heller explains; it just reacts.
When sensory issues appear for the first time in adolescence or adulthood, says Miriam, they’re usually due to some sort of trauma — or the issues would have surfaced much sooner. Knowing that trauma is likely involved helps care providers determine the course of treatment.
And what of longtime sufferers, like Rachel, who struggle for years until a diagnosis finally resonates? What is it about being “sensory” that leads to assumptions of other issues at play, usually either mental or emotional?
OUT OF TOUCH
Psychology, and its diagnoses, have been around much longer than occupational therapy, suggests Rachel. “People are quick to assume that variations in typical behavior and thinking processes are the property of the mental health field,” she asserts. In the ’80s and ’90s, when Rachel grew up, sensory issues weren’t yet common parlance. “That doesn’t mean that many kids like me, who were deemed ‘sensitive,’ ‘needy,’ ‘quirky,’ and ‘particular,’ didn’t have sensory issues; they just weren’t recognized as problematic or challenging — and if they were, it wasn’t always clear what should be done.”
Further, kids don’t always know the right way to explain their feelings. As a child, Rachel didn’t have the words to say, “When we’re outside, especially in the middle of Manhattan [where she grew up] and especially at night, the bright lights and the big buildings and the unexpected sounds make my body feel as if it’s detaching from my brain, and suddenly everything looks sharp and split into so many little pieces, and I feel like sounds are painful and I get trapped inside my head, and so my palms sweat, and I feel like I can’t connect to my body or my surroundings anymore.”
Because Rachel couldn’t convey the depth of her sensitivities in many situations, her parents saw only the related post-exposure behaviors, like tearful meltdowns when she was overstimulated. “I was known as a very sensitive kid who cried very easily. But many kids are sensitive and many kids cry.” (And lest anyone think otherwise, she adds, “I grew up in a loving family — I’m certain that if my parents had understood the degree of what I was experiencing, they’d have reached out to the right people sooner.”)
Children also have no reason to suspect their peers feel anything differently from them. It’s only as they mature and their fluctuating hormones make it even more complex to process sensory input that they realize that not everyone feels this overwhelmed, this bothered, by that sound or that smell.
But even psychologists and medical professionals often misdiagnose the hyperactivity, anxiety, depression, or stress relating to sensory processing difficulties as psychological in origin, rather than sensory. Rachel’s doctors thought so (even Rachel herself did) and at one point, diagnosed her with panic disorder. True, anxiety disorders and depression are common secondary diagnoses for adults with SPD, Rachel says, but they don’t always exist on their own. Some are SPD in disguise — “One person’s discomfort having food in their mouth can look like an eating disorder while another’s swinging moods can look like a personality disorder or a mood disorder” — and some are hardwired patterns from decades of misunderstanding.
Now, Rachel is passionate about SPD and how it affects adults, and advocates for them. Viewing SPD as a childhood disorder, she writes, “fails to recognize the innumerable adults who lacked a proper diagnosis in childhood, and must now learn to redefine themselves and their abilities in adulthood.”
Because adulthood is another story. By the time you’re an adult, you’ve misunderstood yourself — and been misunderstood — for too long, and you’ve built up a world of meaning and emotion around your discomforts and behaviors. You also have familial, social, and work responsibilities that didn’t exist earlier, and you’re expected to perform at much higher levels of functioning.
SENSORY SOLUTIONS
This is why Rachel believes in what she calls the “Tripartite Model of Adult SPD Treatment” — three types of therapy that positively impact adults with SPD or any other sensory processing difficulties: occupational therapy, psychotherapy, and physical therapy.
Occupational therapy is where adults with sensory issues begin their diagnostic journey, where they’re given a diagnosis, put on a “sensory diet” (that includes exercises, tools, and techniques to regulate the senses and the body’s response to stimuli). And as Rachel says, it’s where someone says to you, usually for the first time: You’re not crazy; you’re just wired differently.
The modalities employed by occupational therapists depend on many variables, says Miriam, such as a client’s exact symptoms, needs, age, environment, or risk factors. There is the standard sensory integration work, which focuses on helping the body integrate sensory input, like the noise levels your kids make when they play, for example. Then there’s reflex integration, which tests for retained primitive reflexes and encourages reflex integration, or easing reactions to sensory information so one reaches a functional level of performance. Chava Zehava, for example, will often turn to modalities of treatment such as Rhythmic Movement Training, and the Masgutova Neurosensorimotor Reflex Integration (MNRI®) method, a model of treatment developed by neurodevelopmental researcher Dr. Svetlana Masgutova, and proven, based on abundant empirical evidence, highly successful in helping adults reintegrate primitive reflexes.
How effective is occupational therapy for adults? There are two main goals, says Miriam: The first is teaching a client to modify her environment so it suits her particular needs. The second goal is treating the symptoms and helping the person become more adaptable to the environment. Often the former is given more attention, either because the latter isn’t believed to be reasonable (especially for adults whose brains are no longer as elastic) or due to lack of tools and resources. But Miriam is particular to maintain a 25%-to-75% ratio with clients, where she focuses more on the long-term goal of helping people become more adaptable. Not only is it possible, she posits, but it may be more realistic than expecting to change one’s environment.
The emotional component to sensory processing difficulties is not well-accepted, says Miriam, nor is the idea that the emotional aspect can be addressed through OT. As Miriam is chair of legislation for the New Jersey Occupational Therapy Association, she’s had to lobby at the state level for OTs to be recognized as practitioners of the healing arts. Sufferers can still seek psychotherapy, both Miriam and Rachel urge, because there is usually more than just sensory symptoms to deal with, and the combination work can be very effective.
Psychotherapy, professionals believe, helps with secondary, related diagnoses, as well as learning to accept yourself the way you are. As a trained mental health counselor, Rachel is a proponent of mental health care, especially as part of treatment for sensory processing issues. While you can’t un-think SPD, as she likes to say, “you can learn new ways of approaching the secondary anxiety or depression. You can uncover better methods to cope with the feelings of shame, guilt, embarrassment, and worthlessness that often accompany it when it’s gone undetected for so long. You can work on trauma. You can learn to love yourself and your differences, and see them as unique strengths that make you — you.”
Rachel also believes in the effectiveness of some forms of physical therapy for strengthening individual senses, especially vision therapy, which she says can be very powerful for people with visual sensitivities.
Do any self-help techniques or at-home strategies exist for people looking to implement more immediate change and perhaps save money?
There are many ways to nourish the nervous system so that it doesn’t get so quickly depleted by sensory overload, believes Dr. Heller, whose own experiences as a “sensory defensive” are proof of the effectiveness of these techniques. Carefully planning and implementing a sensory diet is foremost, says Dr. Heller. Include activities that offer powerful and long-lasting effects on your nervous system, like movement and exercise. Set up your environment wherever possible so that sound, light, and odors are at a comfortable standard. An organized, aesthetically colorful environment, in which temperatures are well modulated, is equally calming. Strive to eliminate anything that will do you harm — like toxic materials, stressful lighting, and unnerving noise.
Dr. Heller also talks about eating the right foods and deep breathing. Maintaining the correct posture is also helpful, as are different types of hands-on bodywork, like craniosacral therapy, massage, or touch therapy. For anyone with sensory difficulties who can tolerate touch, Miriam recommends twice-weekly full-body massages by a massage therapist, for 60-90 minutes at a time. And, she says, “make sure to specify whether your preference is for light touch or deep touch.”
Even for those who aim to self-therapize, professional advice in planning it out is often invaluable to identify areas of difficulty and ensure that changes only benefit the individual.
BEING YOU
There’s little lonelier than suddenly realizing what you’ve been struggling with all along, and not knowing what comes next, says Rachel. The realization, she says, is an “aha” moment itself; you admit the very thing you’ve been struggling to both hide and define, and that feels powerful. But it’s accompanied by the frightening question of “What now?”
“Now,” says Rachel, “you get to reach out and join the community of others just like you, who can commiserate with you and laugh with you about your challenges and quirks. Find an OT who works with adults, and look for a psychotherapist who understands the complexities of neurological conditions.
“And know that it’s okay to be different. It’s okay to be you, exactly as you are. It’s okay to have boundaries and limits that, when crossed, make you feel sick, and it’s okay to stick within the parameters of your comfort zone as you gently nudge them outward at your own pace. It’s okay to have trouble transitioning from event to event, to crave deep squeezes, and to avoid fluorescent lights. And it’s okay to have shutdowns or meltdowns and question your abilities.”
Because you are who you are. You can resent and fear your differences, or you can embrace your challenges and live your best life.
Thanks to Raquel Bondar, OTR, of The Thrive Group; R.P.; and R.C.G. for their contributions to this article.
(Originally featured in Family First, Issue 600)
Oops! We could not locate your form.