Picture Perfect?
| January 2, 2024How the ultrasound made it to the big screen in medicine

Bashie Lisker with Yonah Chatzinoff
Ultrasounds have gone from shipyard tool to medical standard. But when it comes to using them for prenatal care, there’s still some societal skepticism. Why is that? A look at the story behind the screen
G
ila was expecting twins in an otherwise uneventful pregnancy. At 27 weeks, though, the ultrasound technician had a stricken look; the conversation that followed with her obstetrician was even more unsettling, with her doctor gently telling her that one of the babies was unlikely to survive. While in turmoil, Gila sought guidance from a mentor, and got even more confusing information. “Ultrasounds aren’t the be-all-end-all,” she was told.
Gila’s mentor had a family member who, 20 years before, had been through a similar situation. The mother was told that one of her twins had no heartbeat. But the ultrasounds were wrong. Two healthy babies were born, and the mother had spent months of her pregnancy in painful grief for nothing.
“You can’t rely on a miracle, but don’t lose hope completely,” Gila was told. Looking back, she isn’t sure if it was the right or wrong thing to hear. The distressing prognosis was an incredibly difficult burden to carry through the third trimester — visiting the doctor, hearing the dire warnings each time — and that sliver of hope left her simultaneously encouraged and devastated. Could it be just a question of emunah? At what point was she relying on a miracle? Should she be preparing herself for the worst? Again and again, Gila found herself wondering: Could she really rely on those grainy images on the screen?
Gila’s mentor is not the first to cast doubt on the effectiveness or accuracy of the ubiquitous ultrasound.
Ultrasound imaging has come a long way since the false-alarm story Gila’s mentor had experienced. But rumors about its accuracy still persist, leading some women who otherwise embrace first-class medical care to feel apprehensive or distrustful of, or even avoid prenatal ultrasound screenings.
Perhaps it has to do with the ultrasound’s historical lack of reliability.
To put it simply, ultrasounds use sound waves to show a picture — the sonogram. The very first ultrasounds were used in shipyards and industrial factories. Researchers sometimes used ultrasounds to analyze the human body, though the subjects had to be put into a pool of water to get a decent picture. A huge breakthrough came in 1955, when Dr. Ian Donald took the ultrasound machine at a patient’s workplace — used to find flaws in metal welding — and used it first on human tissue and then on a piece of steak to test if it could read the differences. It passed with flying colors.
From there, he developed an ultrasound that would work with a sensor pressed against the abdomen through a layer of olive oil. Messy, but effective, and it changed pregnancy health forever. Pat Anusas, a midwife who witnessed an early pregnancy ultrasound in the 1960s, talks about watching her first scan, as quoted in Smithsonian Magazine (Winick and Fisher, 2021). “I still to this day can’t believe what I saw… didn’t know if it was going to work or not — but it did work. And both the mother and I were so excited — she couldn’t believe she could see her baby.”
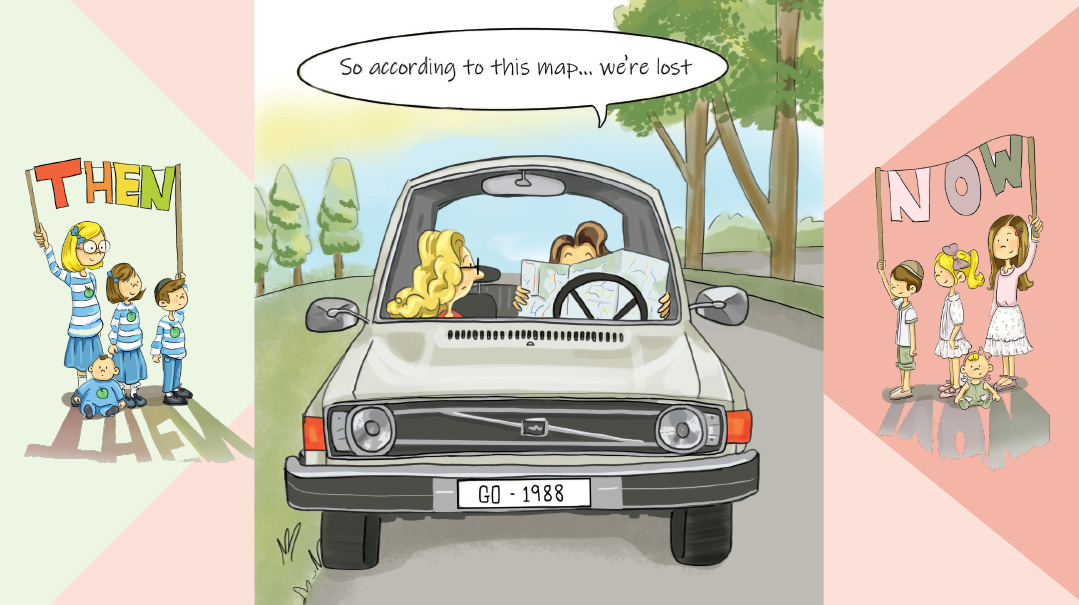
It wasn’t until the 1980s that ultrasounds produced scans that we would recognize today, showing the movements of the baby and some recognizable features. But even those scans were weak and vague. Joan Altman-Neuman, OB-GYN, of Hewlett, New York, remembers doing scans during that period, when the machines were so simple any doctor could easily read them, and there wasn’t much to see.
They were also notoriously inaccurate. In 1992, my mother went to a doctor, just a few months postpartum, sure that she was expecting again. The at-home test confirmed it, but the blood tests were inconclusive. “You can get a sonogram,” the doctor offered. She traveled some distance to get a scan from a brand-new, state-of-the-art machine. “You have a cyst in your uterus,” she was told. “We’ll need to schedule an extraction.”
She begged her doctor for one more look. Finally, he used a Doppler (a small machine that uses ultrasound waves to produce sound instead of an image) to listen to her abdomen — and found a heartbeat. The “cyst” is now a mother herself.
Modern ultrasound machines need to be operated by specialized technicians who produce detailed descriptions of the baby’s anatomy and spot anomalies, for better or for worse. Many of those anomalies are nothing — ordinary issues that go away within weeks. Despite this, Heather Caudell, RN, CNM, a midwife who practices in a traditional OB-GYN clinic in Texas, is firm in her belief that it’s better to be informed in this case. “Most patients appreciate and value the information that we find,” Heather says.
But the wrong information or a poorly relayed possible finding can cause stress and fear. When we have all the information but lack context, especially in a heightened emotional state, we can get hung up on minor details. One doctor tells me that there’s a common cyst seen in the brain on anatomy scans that goes away within a few weeks. It can be a sign of chromosomal defects when paired with other findings, but on its own, it’s not a problem. Still, patients often panic and there’s lots of anxiety.
Late in pregnancy, pre-birth weight estimates remain notoriously unreliable. “Sometimes, we need to know how large a baby is to decide if we’ll have to do an induction or a cesarean section,” Dr. Neuman says. “We have charts of acceptable weights, but sometimes we forget that edge percentiles are fine, too! The danger is that when we can see everything, we can start looking for problems.” My oldest son, I was told, was 13 pounds and counting, and I was scheduled for a cesarean section the next day. When he emerged as a healthy eight-pounder, it was a bit of a shock.
To Know or Not to Know
I remember sitting with my own doctor before the nuchal translucency scan, an optional procedure done between weeks 11-14 of pregnancy, used to screen for Down syndrome. We discussed the pros and cons. Ultimately, knowing that my child might have Down syndrome wouldn’t affect my medical plans or my feelings about the baby. But I liked the idea of being aware, of having months to adjust to a more complex infancy instead of getting the information postpartum with a baby in my arms.
Heather shares her perspective as a provider, when she recalls delivering several babies with Down syndrome after the mothers had declined testing. In one case, the mother quickly shifted from denial to acceptance. But in the other, the mother was shocked and angry. She refused to hold or feed the baby during the first few hours after birth. “Some women want knowledge so they can mentally prepare,” Heather says.
Meira disagrees. When she was expecting her oldest child, over 12 years ago, she was told her baby would likely have Down syndrome after an early scan. She declined an amniocentesis to confirm, concerned that she’d be putting her pregnancy at risk, and discovered after birth that the diagnosis was an error. For her next few pregnancies, she avoided ultrasound screenings. She felt that the anxiety took away from her pregnancy experience. Looking back, she realizes that her provider could have phrased his assessment more carefully; but at the time, she spent significant emotional energy bracing herself for a challenge that ultimately didn’t come.
A Matter of Safety
There are also safety considerations. Years of research back the safety of today’s medically indicated ultrasounds done by trained providers. But the American Institute of Ultrasound in Medicine continues to recommend they be performed using the ALARA principle — using ultrasound exposure “as low as reasonably achievable” to gain the necessary information. For this reason, 3D “souvenir ultrasounds” are not approved by the FDA or other medical organizations. The machine being used in your doctor’s office has been carefully calibrated for its purpose, and the ultrasound protocols have been thoroughly considered by experts.
To get a sense of any potential risks, we spoke to a biomedical engineer who specializes in ultrasounds. “My background is in therapeutic ultrasounds, when we intentionally damage tissue in order to treat medical conditions,” he explained, quickly identifying why some may be concerned to have ultrasounds done in pregnancy. However, he went on to explain the differences between his methods and diagnostic ultrasound.
First, he broke down the various ways diagnostic imaging is performed on the body. He started with radiologic imaging such as MRI and X-ray, both of which use light waves, or electromagnetic energy. “There are a few kinds of radiation used in medicine. With the high energy level (or frequency) of X-ray or CT, each light wave can damage a strain of DNA. But with an MRI, operating at a much lower frequency, there isn’t enough energy to damage anything. It has less energy than sunlight, or even a light bulb.” He listed examples of energy across the spectrum. At the very bottom are the low levels that run through electrical lines. MRI ranks far below visible light, and X-rays ranks far above, though below the level of radiation used to treat tumors.
Unlike true radiologic imaging, ultrasounds use sound waves instead of light waves. With light, the higher the frequency, the more energy it has, and the greater the damage it causes to DNA. With sound, there’s no relationship between frequency and energy. Consider the vibration you feel when someone hits a bass drum — that’s sound traveling at a very low frequency. Ultrasound uses a higher frequency but isn’t more powerful; any risk of damage is purely mechanical. At a therapeutic level, those sound waves can be used to break up kidney stones via micro shockwaves. But imaging ultrasounds use so little power that they can’t do any damage.
A secondary concern is heat. “Focused ultrasounds create heat because the sound waves are moving so quickly that they cause friction in a small area. But when you’re doing a pregnancy ultrasound, it’s done in small slices, with the energy spread out enough that there’s no harm to the baby.”
So is there a legitimate concern about the safety of ultrasounds? Much research has been done, and no studies have connected standard pregnancy ultrasounds to any bodily harm. One study linked certain ultrasounds in pregnancy with left-handedness in boys. Another study done on mice led to the guideline to avoid contrast agents in ultrasounds. A Lancet study compared women who only got the standard anatomy scan with women who got many more scans, especially early in the first trimester, and found some evidence that women in the latter group delivered babies with slightly lower birth weights. That study informs some of the guidelines on when to do ultrasounds, including a recommendation to simply show the heart beating on a very early scan without using the Doppler on the machine to listen in.
He reiterates what we learned during our research for this article — all medical organizations recommend against getting souvenir 3D ultrasounds. Ultrasounds should be used sparingly and only in the hands of experienced technicians. While they have never been known to cause damage, after decades of use in millions of women, they do hold the potential to cause harm and should be used only when there is a benefit to outweigh even a purely theoretical risk.
A Lifesaver
Avigail was shocked when the doctor called her in after the 20-week anatomy scan. The bad news came quickly: Her baby had a cardiac defect. For the next five months, she would be in a state of limbo, worrying about the heart issue of a baby whom she couldn’t yet take care of or touch or even know by name.
At that point, the doctor sat her down and walked her through her options. “This is the best time to learn about the problem,” she reassured her. “It means we’ll be prepared.” Avigail met with a pediatric cardiologist and thoracic surgeon. At delivery, the head of the NICU was in the room and immediately took control. There were no surprises when the baby was born; instead, the entire surgical procedure was set up and ready to go, and the baby was safe and healthy soon after birth.
“Having that set up prior to delivery can save a baby’s life,” says Joan. “Instead of having to figure out why the baby is turning blue, testing, and explaining the situation to the parents — and all the things that would have taken a lot of time with a very sick baby — all of this was done before the baby was born. The nursery was ready, the heart surgeon was ready, and the parents were prepared both informationally and emotionally for what came next.”
Dinah Waranch, RN, CNM, a certified nurse midwife who attends out-of-hospital births in Dallas, takes a more relaxed approach when asked if every woman should have ultrasounds during pregnancy. “Every woman should have autonomy to make her own decision based on the risks and benefits. That’s standard of care in midwifery. Therefore, if they opt out while understanding my description of risks and benefits, that’s okay.” There are cases when she strongly advises it, of course. If there is a question on a due date, she recommends an early sonogram, and she does believe in the benefit of an anatomy scan.
In other cases, she’s less enthusiastic. “People will ask for sonograms at other times in the pregnancy just to see the baby or check that everything’s okay. I want people to make choices, but I certainly don’t encourage it.” This creates more anxiety in patients. She also notes that there are many places that will do unnecessary ultrasounds just so the practice will profit more from Medicaid patients.
Heather believes that every woman deserves at least two ultrasounds in pregnancy. Early on, the ultrasound can be crucial in finding an ectopic pregnancy, when the pregnancy happens outside of the uterus and can be life-threatening if untreated. She also reiterates that the 20-week anatomy scan is vital to find defects. “If a baby has a condition that needs to be monitored, it’s better that the mother knows and is mentally prepared.”
Most medical professionals recommend only two or three major scans for all women. The first is early on, to establish a due date and a viable pregnancy. Joan likes to do an ultrasound at the first visit. “We now know that fetal morbidity increases after 41 weeks, so we need to know the right due date. Ultrasounds done before ten weeks are extremely accurate.” The second is at about 20 weeks. That’s the big anatomy scan. There might be a third scan near the end of pregnancy to check on the brain and the baby’s positioning and weight before delivery.
Joan won’t see patients who decline ultrasounds. “Knowing what to expect can save a baby’s life,” she says flatly. “Plenty of patients might tell me that knowing won’t change anything for them, so why should they get an ultrasound? That’s not relevant. What’s relevant is: Is there a problem? What can we do about it? That’s the purpose of the ultrasound.”
Gitty Bodner, an ultrasound technician, advocates strongly for the later ultrasound. “It can tell you which hospital to go to that has specific doctors who know how to deal with these things.” Heart defects in particular come up. “If you know about it right away, it can save babies.” She also mentions a prenatal procedure that can help in twin-to-twin transfusion syndrome, in which twins sharing a placenta both fail to thrive. As the later scan becomes more productive and helpful, she says, more chareidi rabbanim have begun to advise the scan.
Gitty remembers a woman who came in for a routine checkup, and the ultrasound indicated that the baby wasn’t moving at all. After time and a bite of something sweet, nothing had changed, and the doctor ordered an ambulance and an emergency C-section. The baby was born with the umbilical cord wrapped tightly around its neck. Just a few more minutes might have made the difference between life and death. (She clarifies that spotting the umbilical cord around a baby’s neck can be a normal finding in the absence of other indications of a problem.)
Spiritual Considerations
For some there is an inyan of “tamim tihyeh,” of leave future things for the future, and even that is open to interpretation. Reb Henoch Leibowitz of Yeshivas Chofetz Chaim advised his talmidim not to find out the gender of the baby, no matter what. That’s not “need to know” information. However, any information that would be used to preserve the health of the mother or child could be screened for with ultrasound.
Bat Tzion Kronenberg, a nurse, feels that women should first ask their rav before declining an ultrasound. “I ask the women why they’re declining, and the most common response is just that they’re not supposed to, but most never asked for a psak.” Some of the women remember that their mother didn’t get a scan, and some have just heard from others that it isn’t done. Few of them have recently consulted a rav. “I explain that things have changed tremendously over the years, and it’s important to actually ask your rabbi, or ask a rav who’s a maven in medical halachah and its application.”
“There is no halachic prohibition in performing an ultrasound that doesn’t endanger the mother or fetus,” says Rabbi Popper, an advisor and posek at Machon Puah in Yerushalayim, as well as a senior genetics counselor in Hadassah Medical Center. “But for some rabbanim, there is an ideological consideration.” The still-lingering fear, for some rabbanim, is that an ultrasound can reveal a defect that can’t be fixed. Rabbi Popper quotes several gemaras, the gist of which is simple: If we don’t know the degree to which we are afflicted, we don’t have to rely on a miracle — and we can therefore depend on Hashem’s salvation.
But like the other medical professionals in this article, Rabbi Popper is quick to provide a number of stories in which ultrasounds proved very beneficial. He points out that ultrasounds have changed and developed and that today, much of the time, we aren’t simply looking at those suspected untreatable defects and waiting to see the outcome. “There are many cases when we can use sonography to manage the pregnancy. The ability to diagnose does sometimes allow for intervention during pregnancy. Of equal importance, having the right medications on hand and choosing the place of birth based on the availability of surgical options can be critical in saving the baby’s life.”
Here’s where the dilemma lies. For every tragedy, there are a dozen more situations that can be remedied or addressed, either before birth or right afterward. When we avoid the possibility of thwarting a neis, which we know from Chazal comes more easily to hidden places, do we also keep ourselves from teva — from all the natural tools and science that Hashem gives us to heal? Each woman has a unique perspective, to be explored with the input of her rav and spouse.
My fourth pregnancy ended in a late miscarriage. I had a lot of fear going into my fifth, compounded ten weeks in, when I thought I’d miscarried again. The ultrasound revealed that the baby still had a heartbeat, but she was sitting right next to a large hematoma. The doctor didn’t reassure me — what purpose was there in reassurance when we didn’t know if the baby would be all right? I found it difficult to settle in to the idea of being pregnant and hopeful.
Eventually, I was able to feel the potential and possibility of the baby’s survival. At 24 weeks, the baby still seemed healthy, and even my doctor was able to tell me to relax. As much as the ultrasound had filled me with dread, it was also my comfort. Every time I would see that the baby was growing and developing well, I was reassured that she was doing okay despite any ongoing risks.
When my daughter was born, I was able to feel the miracle more closely than ever. I’d been positive that I had lost her, and now she was here in my arms: fully formed, healthy, and beautiful. After the faith that sustained me throughout my pregnancy, it was easy to choose a name. We called her Emunah.
Ultrasound’s Other Uses
As a noninvasive way to look into the body, ultrasounds also shine as a diagnostic tool outside of pregnancy. Ultrasound is used to assess organs within the pelvis and assist in fertility diagnosis and treatment. While ultrasound waves don’t travel well through bone, and even more poorly through air, modern ultrasounds can generate clear images that doctors use to both assess and treat soft tissue, muscles, and fluids throughout the body. Ultrasound can be used to identify kidney stones and even break them up into fragments with intense sound waves.
When there is a concern of a blood clot in the leg or a growth or narrowing of arteries in the neck, ultrasound is used to examine the speed and direction of blood flow. Echocardiograms to check the heart and ultrasound-guided biopsies of tumors are some of the more well-known uses. Ultrasound is also used to diagnose appendicitis, to assist in the placement of epidurals, treat cataracts, and even to decrease pain and speed healing in arthritis and injuries.
In newborns, ultrasound is used to assess for congenital defects of the hips. In some countries, this is universal; in others, family history or a breech position during pregnancy will determine whether ultrasound will be used. If there is a concern regarding a newborn’s brain, ultrasound can be done while the fontanels (soft spots) are still open so there’s no need for radiation. Ultrasounds, especially to the abdomen, are also done postpartum if something concerning is found during pregnancy.
Just as ultrasound use moved from the shipyards to the obstetrician’s office, it continues to develop wider and wider applications. Focused ultrasound is a new way to perform “surgery” without ever having to cut through the skin, and is used in treating uterine fibroids, prostate cancer, and essential tremors. Research is being done on how ultrasound can be used to improve the delivery of medications, especially to the brain, and with microbubble tracking that follows medication through the bloodstream.
Yonah Chatzinoff, RN, WHNP-C, is a health consultant who lives in Israel.
(Originally featured in Family First, Issue 875)
Oops! We could not locate your form.