Not By Accident
| August 19, 2025Kashi Grossman is a detective. Her mystery? The inner workings of the bedwetting child

Kashi Grossman, OTR, gives occupational therapy, encouragement, and practical steps to families with children who struggle with bedwetting and a lack of control over their basic bodily functions. In a situation that causes deep isolation and shame, Kashi Grossman is the warm, professional harbinger of hope.
Answering the Call
Esty’s* eyes reflected utter desperation.
As a pediatric occupational therapist based in Passaic, NJ, for over three decades, I worked with hundreds of children in public and private schools in my area, as well as a local sensory clinic. The kids I saw on a daily basis ranged in age from preschool through high school. Esty was one of the mothers.
At the clinic, we had recently noticed a troubling phenomenon.
“Do you notice that some of the kids smell?” one of my colleagues asked me hesitantly. We compared notes and realized that it was very prevalent. And not only that, but some of our patients were also constantly wet, clearly from involuntary accidents. We were working on so many different areas with the kids, but somehow, we’d missed this crucial piece. So when a colleague mentioned that she was taking a course for OTs and PTs on pediatric bowel and bladder conditions, I decided to sign up. It couldn’t hurt to know a little more about something affecting so many youngsters I saw every day.
During a therapy session with Moishy, one of the older boys in the practice, I casually mentioned to his mother, Esty, that I was taking the course.
She looked at me, her face taut with strain, and finally whispered, “We have problems.”
I was shocked — both at the idea that this big boy still struggled with such issues, and at the raw desperation etched across his mother’s face. It was a cry for help echoing through the silence, and I suddenly knew that I wanted to answer that call.
To Save a Family
I needed to know more. That initial course became another and another, as I devoured the knowledge and insights of experts in the field of pediatric bowel and bladder conditions. Vistas of understanding opened, and I began to find my place as a pediatric OT in this incredibly complex field.
Toileting is such a natural function, yet it requires the smooth synergy of an unbelievable number of body parts, muscles, nerves, and senses. While a physical therapist focuses on the physical component — the strength of the muscles involved — an occupational therapist examines the senses that detect fullness and the urge to go to the bathroom, and whether the body’s basic reflexes are working properly. All of the above are crucial pieces to successful toileting, both during the day and at night. When one component isn’t working properly, it’s a recipe for frustration, shame, and despair.
Since it’s not a topic people normally discuss, bladder and bowel issues make children and families feel isolated and completely alone. Mothers and children are often reluctant to open up and ask for help, and as children grow older, I see them become progressively more embarrassed and ashamed.
Dr. Steve Hodges MD, a world-renowned urologist, explains that when children lack these basic functions, they have fewer friends, and they’re limited in where they’re willing to go (how can a bedwetter attend sleepaway camp?). The entire family suffers.
Esty’s story echoed Dr. Hodges’s predictions. She told me that her world had become unbearably lonely. Her son had constant accidents. She hesitated to go out with her children for fear that he would have an incident in public. She was constantly fielding calls from school about accidents, and the topic consumed her family’s life.
And Moishy — old enough to understand, and subjected to the taunting of classmates — was carrying the psychological burden not only of his shame, but of his family’s. According to Dr. Hodges, the harshest consequence for chronic bedwetting and leakage is a higher rate of trauma and suicide among children who cannot control these basic functions.
I knew I had to try to help Esty and Moishy and all the other suffering families who would eventually find the courage to come to my office. I began dedicating my time to children struggling with these challenges, and I also welcomed their parents — because when I help a child, I know I’m also saving a family.
To Save a Child
For some parents, toilet training can be a nightmarish ordeal. It’s never easy to lock horns with a stubborn toddler who isn’t interested in giving up diapers. But for families where toilet training never seems to end — where children are bedwetting long past ages three and four, or experiencing leakage during the daytime — there doesn’t seem to be light at the end of the tunnel.
As a pediatric OT specifically trained in bladder and bowel issues, I’ve learned that the reasons for such problems involve a staggering array of our bodily senses.
There’s the tactile system, which allows us to feel sensations — wetness, pain, pressure. The proprioceptive sense helps us “know” where our bodies are in space. I once worked with a child who had very low proprioceptive awareness. He had low muscle tone and a weak core. Whenever he came to my clinic, I would wrap an abdominal binder around his waist, and suddenly he could “feel” where his body was and could successfully use the bathroom.
The vestibular sense governs balance and head movement. Some children I’ve worked with actually struggle to balance, making it difficult to sit comfortably on a toilet seat. Without that foundational skill, the rest of the process becomes very difficult.
And then there’s what we call the “eighth sense” — the interoceptive sense — which allows us to understand the feelings inside our body and know what they mean. We feel a sensation, connect it to an emotion or need, and then understand what action to take. Is your heart racing? You recognize anxiety and know how to take deep, calming breaths. Is your throat dry? You identify thirst and reach for water. For a child with an underdeveloped eighth sense, this connection is surprisingly elusive.
Kelly Mahler, a well-known OT, once described a young boy who couldn’t interpret what his body was telling him. One morning, he said to her, “I feel like I have a gallon of milk in my belly!” Clearly, he needed to use the bathroom. But when Mahler asked, “So what should you do?” the boy just shrugged. He could finally identify the sensation, but he didn’t know how to respond.
Basic weakness in a child’s core, or an underdeveloped rib cage, can prevent specific muscles from working correctly, leading to constant accidents. This was the case with a child I once saw in my clinic. His physical therapist used exercises to strengthen his core for walking, while I strengthened his core to help with toilet training. Baruch Hashem, we were both successful!
Detective Drama
With so many variables at play, saving a child (and the family) isn’t always straightforward. My job is to hunt down clues, to be the detective piecing together the puzzle to determine how to make it all fit together properly.
Some parents come to me without having tried many alternatives. Others show up as a last resort, having exhausted every option they could find. Day training, night training, leakages — I’ve dealt with them all.
When a parent arrives with a child in tow, I start with some basic clues:
- Is your child constipated? This is a huge factor. Full intestines press on the bladder and cause leakages. An X-ray can help reveal what’s happening inside. (And no, constipation doesn’t mean throwing MiraLAX at the problem and hoping for the best, but that’s a topic for another time….)
- Does your child snore? Snoring indicates an upper respiratory obstruction. In simple terms, something is stopping enough oxygen from reaching the brain. When the brain lacks sufficient oxygen, it can’t properly receive the “I’m sleeping” signal, and the body eliminates waste as if it were awake. This clue often involves consulting an ENT specialist.
- Is your child bedwetting within six to ten months after daytime training? That’s still within the normal window. After that timeframe, there’s likely an underlying issue. While it’s possible for young children to outgrow bedwetting (He’ll just outgrow it, right?), there are many reasons they don’t.
- When your child uses the bathroom, are their feet properly supported? For young children whose feet dangle, using the bathroom can feel scary and unstable. Consistent foot support is a simple intervention that can make a big difference.
- Do you know when your child wets the bed at night? Sometimes, a simple schedule reset can help. If your child typically wets the bed around midnight, try waking them at 11:45 to use the bathroom and see if they stay dry.
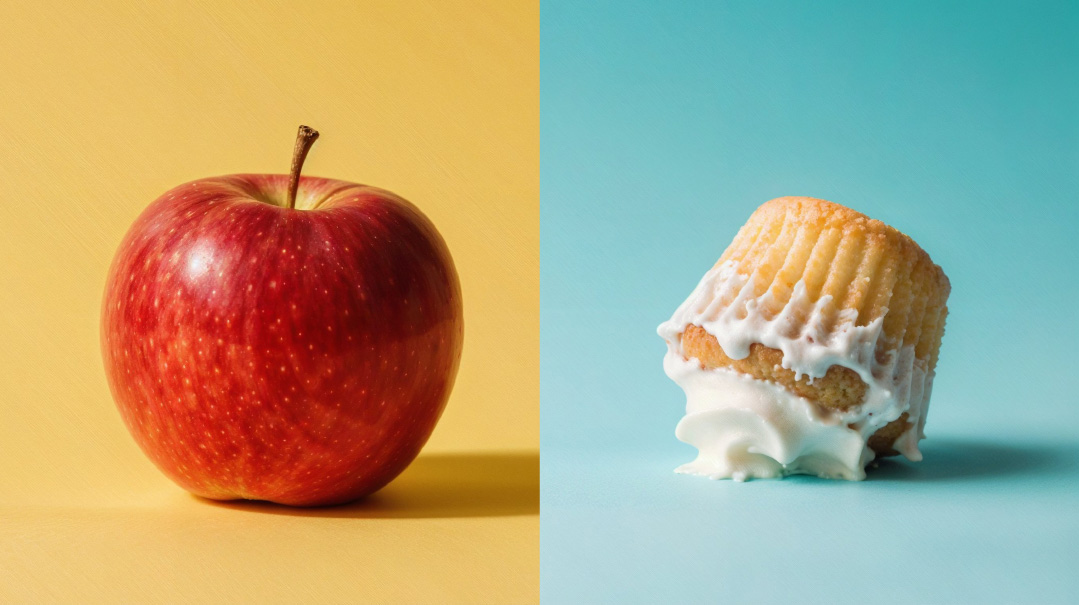
- Is your child consuming bladder irritants before bedtime? Coffee, tea, soda, alcohol, chocolate, acidic fruits, dairy, and spicy foods can all cause children to need more frequent bathroom breaks. And while most children aren’t sipping a rare French vintage before bed, a glass of milk can be a culprit.
- Does your child get enough fiber? Fruits and vegetables, plenty of water, and sometimes magnesium supplements help keep all body systems regular.
Keeping a diary — while admittedly a “pain in the neck” — makes it easier to identify patterns and clues. Document everything: when your child goes to the bathroom, when accidents occur, what foods they’re eating, etc. Sometimes, the answers to these case studies show us how we can crack the case.
The Enigma
Even with all our knowledge, all the courses and classes and tests and medications, sometimes we encounter a true enigma.
One child I’m working with doesn’t have any identifiable physical problems. She’s a healthy, normal child who simply has little control over her basic bodily functions. All her tests have returned normal results, and her doctors are completely baffled.
But we’re not giving up. We’re attacking the problem from every conceivable angle: addressing her core strength, doing daily exercises at home, monitoring her food and drink intake, scheduling bathroom breaks, keeping a diary, and strengthening all her “senses.”
Her parents, major partners in this process, have seen progress, but we have no idea what’s working or why. For now, we’re doing everything possible to give this girl better quality of life, even as she remains an enigma.
And Moishy, one of my first patients? He’s doing a lot better now. It’s been a long road for him, but he no longer has public accidents, and his life has changed completely. So has Esty’s.
I work with so many children who struggle with basic bathroom functions that when I encounter a child who functions normally, I’m filled with wonder. Hodu Lashem! I want to cry when I witness the miracle of Asher Yatzar playing out before my eyes. Do people realize what a gift it is to use the bathroom with ease? Do we appreciate Hashem’s constant blessing?
Elevate
Every day, parents and children come to my clinic, asking, “What’s wrong with me?”
I try to show them that with persistence, hope, and a tremendous dose of siyata d’Shmaya, one day, they won’t have any questions.
Some children have problems I solved quickly and simply; others, like my enigma patient, present ongoing challenges. It’s a humbling, eye-opening experience. But I keep trying. The satisfaction of seeing the light dawn in the eyes of a child who knows they can finally control their body… the hope kindling in a parent’s face when they see that a normal life is possible… they make everything worth it.
- My ideal vacation: an iced coffee, a comfortable chair, and a stack of books
- Recent hobbies: painting and needlepoint (though the needlepoint happens in my spare time, so my last piece took four years)
- My biggest zechus: I have the privilege of videoing Rebbetzin Esther Schwartz and posting her content on TorahAnytime.
*All cases mentioned in this piece are composites.
(Originally featured in Family First, Issue 957)
Oops! We could not locate your form.