Give It a Shot

Is the new weight loss drug a panacea — or a peril?

A
fter Johanna Eichenwald moved to the United States from Morocco, one of the first things she noticed was the different attitude toward food. Back in Casablanca, people made time to sit down for meals, and they were enjoyed with friends and family.
Here in America, she says, people eat and run. There’s also an abundance of kosher food available and so many kosher restaurants, creating a culture of eating highly processed, less-than-healthy foods.
Johanna was slender when she arrived in the US. After she married and began to have children, she put on a significant amount of weight. Over the years, she tried various methods —including the ketogenic diet and juice cleanses — to lose the weight she’d gained. Her lack of long-term success and the prospect of her daughter’s upcoming bas mitzvah prompted her to see a nutritionist last January. She hoped to look the way she had years ago in time for the occasion.
Her nutritionist’s program resulted in some weight loss, but the progress was slow. She was losing only one pound a week. “What do you do when you want to lose a hundred pounds?” she asks. “At that rate it would take me two years to lose the weight. It’s a long, hard process.”
Still, she followed the program, until she hit a snag. Delivering mishloach manos on Purim, she wanted a taste of some of the goodies. The cravings were strong. In the short term, Johanna says, a diet is doable, but in the long term, it’s very hard.
“Maybe it’s a matter of self-control, but I don’t think so,” Johanna says. “It’s emotional eating. When you’re young, your parents take that stress. Now as an adult, you have kids, you have bills. I take my comfort from food.”
Then there was the added stress of having all that extra weight and seeing only minimal progress. “Losing only four pounds a month was so frustrating, and so expensive,” Johanna says. She hired a personal trainer to make the pounds melt faster. She built muscle, and while that can be a benefit, it only made her look bulkier.
Johanna, who is 40, is a physician assistant who specializes in hand and plastic surgery at Harlem Hospital. Her patients were the first ones who mentioned the drug Ozempic to her. She’d never heard of it before, but went ahead and researched it.
“It sounded amazing,” she said.
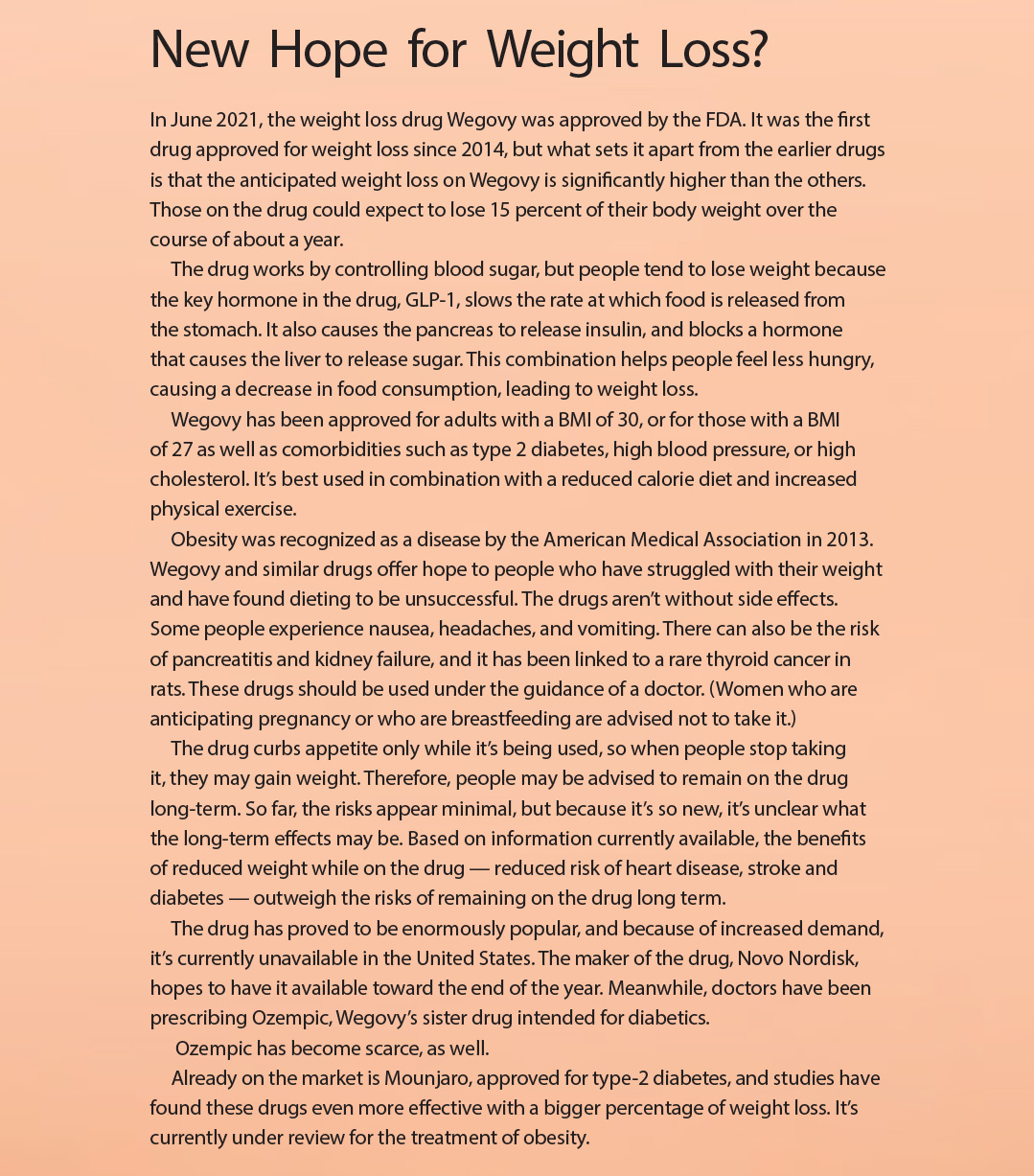
Ozempic is intended to treat type 2 diabetes. People taking it reported weight loss as a side effect. Since then, Novo Nordisk, the company that produces Ozempic, created a sister drug, called Wegovy, specifically for weight management. It has almost the same ingredients as Ozempic, but in higher concentrations. Wegovy’s popularity has made it unavailable, and many doctors have been prescribing Ozempic off label in place of Wegovy.
An Effective Option
Dr. Sheri Rosenfeld, who is board certified in obesity medicine, is an internist with a weight loss practice in Brooklyn. Ozempic and its sister drug Wegovy are effective and safe, she says.
“It’s not candy,” she says, “and some people experience side effects — significant nausea and other gastrointestinal side effects. There is also an increase in gallbladder symptoms and pancreatitis. But for most, it is well tolerated.”
It doesn’t work on everyone, either (only for about 50 percent of people), and some people actually reported weight gain while using it.
For it to be effective, a reduced calorie diet is needed, as well as an exercise program. “When I put people on it,” Dr. Rosenfeld says, “it’s in conjunction with a nutrition and exercise program. I also have them check in with me every two weeks. I’m not recommending that because of the medicine, but because studies have found the more you check in, the more compliant you are with a diet.”
Explaining why she’s in favor of the drug, Dr. Rosenfeld says the medical complications resulting from obesity are worrisome and must be managed. If they can be eliminated, they should. “Obesity is a chronic disease, a lifelong condition that must be managed as much as heart disease. There are multiple downsides to it,” she says. “It puts people at a higher risk for multiple malignancies, diabetes, and hypertension, which can cause heart attacks and stroke. It also causes or worsens osteoarthritis and degenerative joint disease because of the increased weight and wear and tear on joints. Weight loss can actually decrease pain from people’s knee arthritis. This medication is a way to reduce a person’s weight and reduce the medical risks that accompany obesity.”
The medication is FDA approved for long-term weight loss based on a two-year study period, she adds.
Dr. Rosenfeld won’t prescribe it to people with a family history of medullary thyroid cancer, MEN2 syndrome, and pancreatitis. She also says there is no guarantee there won’t be long-term effects because it hasn’t been around long enough.
“There are no guarantees with any medications,” says Dr. Rosenfeld. “As of now we have at least ten years of experience with this class of medication and it has shown to be both effective and safe. We know that not treating obesity puts one at risk, so we have to weigh the pros and cons. We use all kinds of newer medications that don’t necessarily have a long-term track record, but the FDA will not approve meds unless there are studies showing its safety and efficacy. We don’t wait ten to twenty years before a drug is put on the market. And many times, after a drug is in use in the general population, it will be recalled if unexpected complications occur. The US is pretty careful in screening the data on newer drugs before the FDA approves it.”
She doesn’t often prescribe it, because she says that the biggest limiting factor is price. The medication, administered via injection, can cost between $800 and $1,200 per month. In her weight loss clinic, most of her patients are on the lowest dose because they pay for it out of pocket.
“People can’t afford it,” she says. “Insurance companies are not generous in coverage for weight loss. It’s easier to get it for diabetes.”
Although the American Medical Association recognizes obesity as a chronic condition that must be monitored, the government and insurance companies don’t — likely because of the cost the condition’s management would mean to them financially.
A New Me
Johanna met with her doctor to discuss the possibility of starting a weight loss medication. She was referred to an endocrinologist, who recommended she try Metformin, a drug used to treat diabetes, before trying Ozempic. It didn’t have the hoped-for results, so her doctor was ready to have her try Ozempic. First, though, he ordered some medical tests.
“This is my health,” Johanna says. “I wanted to do it the proper way, and not take any unnecessary risks.”
Because of the increased thyroid cancer risk, she had an ultrasound. It revealed a nodule that was biopsied, and proved to be nothing, so she began Ozempic. However, she still has regular screenings — an ultrasound every six months to monitor her thyroid, and bloodwork every three months to make sure there is no change to her general health.
Since starting the medication in July, Johanna has lost 35 pounds.
She’s seen a difference in her professional life. As a PA whose work includes post-bariatric surgery tummy tucks, she has to advise patients to monitor caloric intake to see optimal results.
“They used to look at me as if I was joking,” she recalls.
Many of those patients, who were post-bariatric surgery, would tell her to consider the surgery for herself.
Now she looks different, and she says feels different as well. It feels good to be able to wear something that didn’t fit before, she says. She can put on a new dress, and no one asks her if she’s expecting.
“I used to never shop Black Friday sales,” she says. “Shopping for plus-sizes is always an issue. They never fit well and they’re never on sale. Now I have so many options.”
When she was halfway to her weight goal, Johanna felt confident and motivated enough to give dieting a go without the medication. “I feel like I got that push,” she says. “I’m so happy and grateful for the results.” She admitted to feeling apprehensive about the possibility of losing weight without the aid of the medication. Still, she planned to stick to her diet and exercise regimen.
In for the Long Haul
Rivky is a certified weight loss coach, and she guides many of her clients through lifestyle modifications as they use Ozempic.
“I was never skinny,” she says. “But I never dieted either. I lost weight for my wedding, not because I was fat, but because everyone wanted to be skinny back then.”
She gained 60 pounds over the next eight years, after giving birth to six children. In 2002, she opted to have the band surgery. “I was only 27, and I needed to lose weight,” she says. “It wasn’t going to happen any other way. I was too busy for diet or exercise. My life was stressful enough.”
While the surgery was successful — she lost 70 pounds — she had four more children afterward, and her weight fluctuated.
She was familiar with Ozempic through her professional life, and made the decision to take it when she realized her BMI had climbed to 27. A visit to her doctor confirmed she had high blood pressure, and she was able to get a prescription. She has been on Ozempic since January, and has lost 20 pounds.
“I’ve had no side effects,” she says.
Because obesity is considered a chronic disease requiring lifetime management like all chronic diseases, Wegovy is intended to be a long-term medication. Still, Rivky and others hope to use the medication as a means to help with lifestyle and diet modifications, and their goal is to use the medication short-term. “You use it as a bat to get the ball out of the park,” she says. “Half of my clientele is post-weight loss surgery, and still made the decision to use this drug. The weight loss surgeries and the drugs are not a magic fix. They are only tools, and need to be used correctly to succeed.”
Many practitioners who prescribe the drug say that it helps people make lifestyle modifications, so if at some point a patient decides to go off the medication because of the cost, they have the behavior modification already there.
But Dr. Rosenfeld says that if patients stop the medication, their weight comes back.
“It’s the same as weight loss,” Dr. Rosenfeld says. “Your body works against you. The metabolic rate drops, hunger sets in, and your body pushes you back to those pounds. Of course, weight loss can be done without medicine, but the body will fight against you. Eighty to 90 percent of people who lose weight regain it.”
This proved to be the case for Johanna. After a week without medication, Johanna gained two pounds. She’s back on Ozempic and plans to continue taking it for the next few months. Her doctor advised she continue the drug until she reaches her weight loss goal, and then consider the possibility of going off.
“I was really hoping to achieve the weight loss on my own,” she says.
Caution Required
Although the drugs have the potential to benefit so many, there are concerns. In some cases a prescription is almost too easy to get, and anecdotal evidence suggests people who have no medical need are taking the drug to become ultra thin. Also, because the drug is expensive and currently scarce, people have resorted to below board means of obtaining the drug. This leads to questions regarding sufficient medical oversight of people taking the medication. The problem is that many people taking the drug aren’t monitored regularly.
Avi is a nursing student who works in a clinic in the Tristate area. He has noticed a surge in demand for phentermine, a medication that was approved back in 2011, and is used to lessen appetite. Soon after Ozempic became available, people were requesting that drug.
“Providers are giving it freely,” he says. “And people are taking it because they heard about it from a friend or a neighbor.”
Medicine is a consumer business, he explains. If the doctor won’t give the consumer what they want, they’ll go elsewhere. “The patient will meet the doctor once, and then there’s no follow-up,” he says. “Or people meet with a doctor via telehealth, and then there is no follow-up at all. People think it’s just a shot. I’ll take it, and I’ll lose weight.”
A patient recently told him he’d been on Ozempic, but was monitored regularly by a doctor. Routine bloodwork showed an abnormality, and further testing showed a mass in the patient’s thyroid. It’s unclear if the medication caused it, but it was found because of the bloodwork.
For Avi, this is a cautionary tale, underscoring the importance of medical oversight.
Other providers have told him of cases where patients end up in the hospital after self-adjusting their dose when they think their current dose of the drug isn’t producing significant enough results.
“The patients say, I feel nothing, so they up their dose,” he says.
Avi recently put on 15 pounds, and the provider he works for gave him a prescription for Ozempic. While he is overweight, he doesn’t meet the threshold to qualify for the drug, and he has no additional health problems. He says the drug made him feel horrible. He had heartburn and headaches. He took it for a month and then stopped.
“In theory, it’s a nice concept,” he says. “I lost weight, but once I stopped my appetite came back.”
Avoiding the Real Issues
There’s also concern as to whether drugs like Wegovy and Ozempic will prevent people from getting to the core and foundational issues they have with food. In other words, what prompts people to put on weight in the first place, and once they lose weight with the aid of a drug, will that issue resurface in another form?
Bonnie Giller is a HAES-aligned RD with an office in West Hempstead. She also has a virtual practice, and sees clients from all over the world.
Health At Every Size, also called HAES, is sometimes referred to as a “weight-inclusive” model of healthcare, where weight isn’t considered as one of the most important markers of health.
Bonnie takes no issue with Ozempic as a treatment for diabetes. “I think Ozempic could be a helpful drug for patients with diabetes, which is who the drug was initially intended for. I’ve had patients on Ozempic with very good results,” she says.
However, a drug whose sole purpose is to produce weight loss makes Bonnie uncomfortable. As a HAES dietitian, she does not support weight loss through dieting and restriction. She isn’t opposed to weight loss; she’s opposed to the act of intentionally losing weight through restrictive behavior, such as dieting and calorie restriction.
“Most people looking to Ozempic as a tool for weight loss happen to be long-term dieters,” she says. “On-and-off dieting, weight fluctuating up and down, is harmful to physical and mental health. If they’re looking to Ozempic, it’s really a Band-Aid, another diet, and unfortunately, it deepens their diet mentality.”
She explains that even when people try to make nutrition changes along with Ozempic, often those changes become more rules, and then when they break their rules, they feel guilt, shame, and frustration, and the cycle continues.
“This population of people is really in need of deeper work to recover from dieting and disordered eating,” she says. “I don’t think Ozempic or any such injection is appropriate for these people. I think these are more harmful than helpful. Weight loss is not synonymous with health. Unfortunately, diet culture has hijacked the word health to mean weight loss, and weight loss has become synonymous with being healthy. People need to change their mindset in order to improve their health.”
Research shows that 95 to 97 percent of people who lose weight through dieting and via restriction will regain that weight, and up to two-thirds will regain even more, she says. Even if there are comorbidities, it’s important to treat the individual through a weight-neutral lens.
“Weight loss is not a skill or behavior, but an outcome of habit and behavior change,” says Bonnie. “I have a lot of compassion for those feeling uncomfortable in their body. They feel the only way to become comfortable is through dieting, but there are other ways to take care of their bodies.”
Dina Cohen, a HAES-aligned RD from Lakewood, has seen many clients who have struggled for years to lose weight, and she says that unless people are able to make lasting changes to their behavior, they will inevitably regain any weight they’ve lost.
She also notes that weight loss drugs have been around for many years, and recalls that some of the older drugs were pulled from the market. While there is the hope that the newest class is different, she can’t help but question.
“I don’t know if this drug will be the great game changer people claim it will be,” she says. ”You have to be on it forever for it to work. Once you stop taking it, you don’t have the results anymore. So what happens when people are on drugs for years at a time? Is that sustainable? Will it be effective forever? Will we eventually find out about side effects that outweigh the benefits?”
While she concedes that people with obesity may have other health problems whose risks outweigh the potential adverse effects this drug may have, she says the problem is everyone else.
Dina’s concern is people wanting to take the drug when weight is not a health factor, but when they are taking the drug simply to look a certain way because of societal pressures.
“When you have a perfectly healthy person who wants to take a drug, that is a problem. It’s not a surprising problem, because when it is socially desirable to be a small size, then you have healthy people considering doing things that are not healthy because of the pressure society puts on them. We do a lot of things today to look a certain way. But using a drug to reach an unnaturally low weight is in a different category than a spray tan or false eyelashes. I worry about this becoming normalized in a society where people will go pretty far to get a certain look,” she says.
“Can I see a situation in which people develop a health condition from taking a drug they didn’t need? Or overuse the drug to lose more weight? Yes, I can.” And she has another concern as well — something deeper, and ultimately more damaging, than individuals abusing a drug. “I also worry about how misuse of a drug like this can reinforce the idea that there is only one ideal body size, a size that is unrealistic for most people.”


Dr. Marcy Forta, EdD, MBA is the founder and director of Atzmi, an organization dedicated to supporting the mental health of Jewish girls through programs that improve their self-compassion, body acceptance, and reduce the focus on outward appearances. She specializes in eating disorder education, awareness, and prevention, focusing specifically on risk factors and prevention within the Jewish Orthodox Adolescent Female Community.
(Originally featured in Family First, Issue 819)
Oops! We could not locate your form.