Hidden in Plain Sight
| March 29, 2022Parents of children with invisible disabilities share some of their struggles and tell us how we can make the world a safer, less judgmental place

Parenting in public can be challenging even for the most seasoned parent. Parenting prowess notwithstanding, tantrums and meltdowns are inevitable. But parents of children with invisible disabilities are challenged at a whole other level.
When we see someone with a visible disability, we automatically recalibrate our expectations of how we expect that person to behave. Typically, we’re less judgmental and more accepting of both the child and the parent.
But not all disabilities are obvious. About ten percent of people have some sort of invisible or hidden disability. Many of these conditions are familiar to most people, like autism (also known as ASD, or autism spectrum disorder), ADHD, OCD (obsessive-compulsive disorder), dyslexia, anxiety, and depression, while others, like ODD (oppositional defiant disorder) and Tourette’s syndrome are less familiar. And while people may toss these terms around casually, referring to themselves or others as “a little ADHD” or “so OCD,” these disabilities are real, and affect those who struggle with them in a very real way.
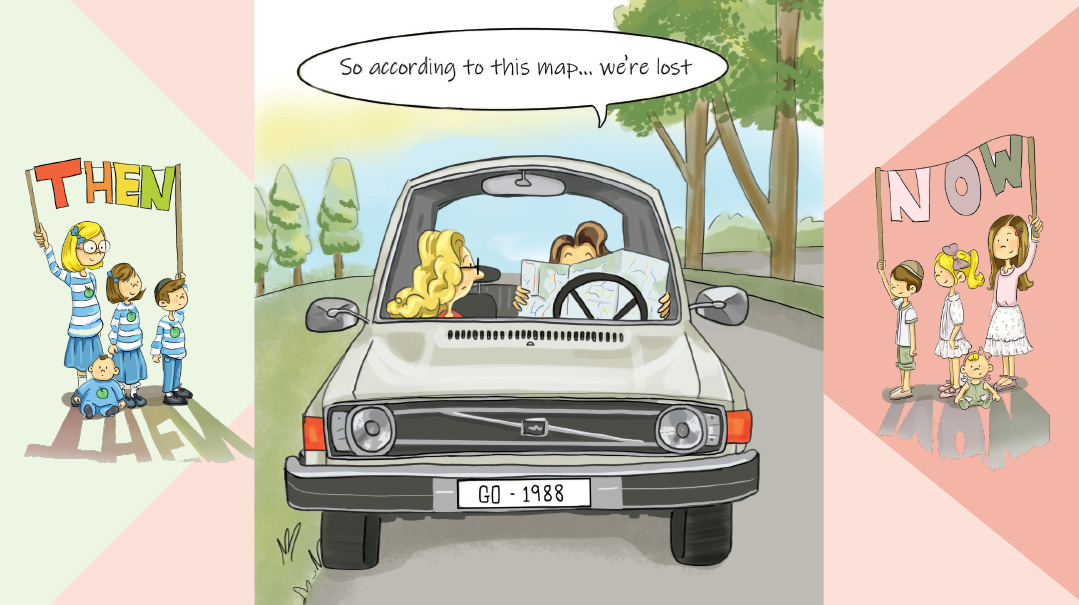
Dassi Shtern, director of special education and SEGULA (an inclusion program) at the Jewish Education Center of Cleveland, which services the local day schools, has worked in the field of special education for over 20 years. “In the ‘90s, the concept of inclusion was rare and misunderstood, and the number of kids with invisible diagnoses was fairly low,” she says. “People are saying ‘Why is there so much ADHD going around?’ But I would argue that invisible disabilities were very much around; people just didn’t know about them, and they weren’t being diagnosed properly.”
Raising children with invisible disabilities brings its own unique set of challenges, not least of which is that these children often look “regular.” They can even behave like neurotypical children — except when they can’t. And when they can’t, the parents are often blamed, by themselves and others, as the cause for this bad behavior.
But these behaviors aren’t simply an issue of discipline. They’re neurological realities. These children are more easily prone to tantrums, meltdowns, or high anxiety, and these behaviors may also last longer than in neurotypical children. They often cannot calm down, and parenting tools or discipline methods that work for neurotypical children can have the opposite result on these children.
Dr. Benjamin Miller, a licensed clinical psychologist who has been working in private practice in the Beachwood, Ohio area for approximately seven years, delivers targeted behavioral, cognitive behavioral (CBT), and dialectical behavioral (DBT) therapies to children, adolescents, and adults struggling with a variety of mental health concerns. He reassures us that “even when the parent is doing everything right — distracting the kids, and having a running conversation, and reminding them of all the rewards they’re going to get for being so good in the supermarket, and the parent is keeping calm and not getting into a power struggle — sometimes, especially with non-neurotypical children, it will become a battle. Even if you’ve done your very best to try to avoid that.”
Far-Reaching Effects
Invisible disabilities have wide-ranging effects on all areas of life, from which shul or school to attend, to how Shabbos looks, and socialization in general.
“I don’t take her into situations when there’s a chance something’s going to come up,” says Baila, whose daughter has autism. “I don’t want her misbehaving, because then she doesn’t feel good about herself.”
“When we moved, people would invite us for meals, and I’d say no,” shares Leah, who has a few children with invisible disabilities. “I couldn’t go with my son. He was a disaster. I couldn’t sit at the table and talk to the adults, I had to always be making sure that he wasn’t making trouble, that he was playing nicely… I couldn’t invite people to our house either, because he would say very inappropriate things at the Shabbos meal.”
Rachel, whose son has ADHD, shared that this year her husband started going to a different, smaller shul. “It’s a place for misfits, almost,” she said. “My husband likes the davening there although he finds it very weird socially. But it works for my kid.”
“It’s hard for her to keep up with her cousins, socially,” says Hudy, whose daughter has Asperger’s, ADHD, and anxiety. “It’s also hard for her to be in a group. One-on-one is easier than when she has to run around with everyone. She gets lost in the crowd. And she always gets left out.
“We were just at a vort, and her cousins were there, and they were just sitting there, not talking to her. Then, another cousin her age came, and the other girls were excited to see her. My daughter is smart enough to know that she’s not included, that they never come here, and they never pick her up.”
En Route to a Diagnosis
There isn’t a clear-cut route to get a diagnosis for an invisible disability, as there’s significant overlap in the behaviors that typify a lot of these disabilities. Is a child unable to focus in class because he lacks the ability to pay attention, because he doesn’t have the necessary executive functioning skills, or is it because he is too anxious to focus?
Shoshana, a mother of eight, most of whom are diagnosed with invisible disabilities, shares. “That’s one thing I feel no one talks about, how difficult it is to get a diagnosis, especially if you have a kid who’s passing his classes and getting decent grades. You can’t get appointments overnight. Sometimes you wait months.”
Even accepting that there’s a problem can be a process. Rachel remembers that when her son’s kindergarten morah shared that her son was more aggressive than other boys his age, she initially dismissed it as “boys will boys” behavior and was very defensive about needing services. Eventually, though, she started paying closer attention to her son’s behavior, which led her to get him assessed.
“When my son’s first grade teacher told me that he had a tic, I thought she was being ridiculous,” remembers Shuli, who has a son with ADHD and ODD. “But she was right. It took me years to really accept that.”
Telling the World
While receiving a diagnosis can provide clarity in terms of treatment options, the path ahead can still be incredibly difficult.
“When a kid in the community gets sick, lo aleinu, the whole community steps up,” Rachel says. “But when my kid with ADHD has no one to play with on Shabbos, there’s nothing. And that kid is looking at a long, hard road of feeling lonely.”
Leah also finds that interacting with others can be painful for her. “I’ve become very antisocial, mainly to protect myself,” she say.
An invisible disability affects the whole family, and different family members will react differently. Leah’s daughter, a typical self-conscious adolescent, found it very challenging to accept her brother, especially when her friends were around. Leah tried to reassure her that most people realize he has special needs, and that her acceptance of her brother would elicit others’ respect.
Leah’s father dealt with his discomfort by preemptively telling everyone that his grandson has special needs, but Leah feels that “sometimes you need to just own your child. You’re proud of him and that’s it — you don’t have to explain to strangers walking on the street.”
Rachel was very transparent with her family. She spoke to different family members privately and gave tips on how to deal with her son’s more annoying behaviors.
She also struggled with the conflict between wanting to share the reason for his quirks with everyone, but also wanting to give him a fair chance to stand on his own.
“My son was so impulsive when he was little,” she says. “That was hard to explain away before he had a diagnosis. Once he had a diagnosis, I wanted to share it with everyone so people would treat him with more empathy … but I don’t think it’s fair for everyone to know your kids’ diagnosis. We need to create a culture of empathy for people who have challenging children, diagnosis or not.”
While parents may want to respect their children’s privacy, keeping a diagnosis entirely a secret doesn’t necessarily work either.
“Humans are judgmental, it’s a reality we all struggle to overcome,” says Dassi Shtern. “How much are we going to let other people’s judgments determine how we help our child? If you’re so fixated on ‘no one can know,’ then you’re holding your kid back because he’s not going to get the tools he needs. Do you want your kid to think that ADHD is bad? That no one can know he has ADHD? Parents have to… be comfortable enough with the situation to truly empower their kid.”
The Medication Conundrum
Many of these invisible disabilities are complex to treat, and parents usually end up doing a combination of therapy, different parenting strategies, special diets, and in some cases, medicine, which itself isn’t so simple. Medication could lose its effectiveness because the kid is going through a growth spurt, or a hormonal change, or it simply stops working.
“Medication plays a huge role in what we see in this population,” says Dassi. “Sometimes you’ll see certain behaviors, and in reality there needs to be a medication change, and medication changes can take months to get right.”
In the interim, parents have to juggle the behavioral fallout while finding the correct new medication and dosage.
Leah has found DIRFloortime a tremendously effective way to connect with her son. “It’s a social-emotional-developmental approach versus a behavioral approach. You’re not looking at them like ‘good behavior — positive reinforcement, bad behavior — negative reinforcement,’ You’re working with a child on his level, getting into his world. It’s very respectful, validating his feelings and growing with him. It works with the child where he’s at, not where he ‘should be.’ ”
Shoshana adds that “so much depends on environment and expectations. In school, [where children] are expected to act like little adults, they drive the adults crazy. But when it’s summer camp, and they’re expected to be wild and crazy, they’re perfect. One son was a counselor at a summer camp for Bnei Akiva, and he had a bunch of really wild kids, and everyone asked him ‘How do you keep those kids in line?’
“And he said, ‘You just get in there, and you’re wild with them and go with it, and you say, “okay everybody we’re gonna do pushups,” and you get it all out, and then you’re like, “okay now we’re gonna sit down, and we’re gonna do the activity.” ’
“Now he’s 29, and he’s a functional adult, he works in nursing home administration. He’s a very hard worker. He does still take medication, which he didn’t start until he was a teen. It changed his life. We had a lot of people tell us that he didn’t meet the criteria for ADHD because he was able to sit and take a test. But medication changed his life.”
The Silver Lining
Despite the many challenges, some parents are able to see the good in the experience of parenting their children with invisible disabilities.
“Parenting him has been a whirlwind of blessings,” shares Rachel
“When he was younger, we lived in Israel in a very affluent lifestyle. I was young and dressed my children in gorgeous European clothing. I was very self-conscious, thinking my kids were my nachas. When you have a child with ASD you learn very fast that we weren’t given children to have nachas, but to work on ourselves to grow together to be better people. My job as a mom isn’t to control my child but to control my reactions to him. That took a lot of work,” says Leah. Today, she says, her goal is to “accept a child for who he is and not who you dreamed he would be.”
“There’s been a lot of frustration and pain and tears, but it’s also been a tremendous growth experience, for me as a person. I see how much closer I’ve grown to Hashem through this process,” muses Shuli.
Dassi notes that “these kids often surprise their parents. I watch the parents struggle, and in most cases it’s the parents of the kids with invisible disabilities who seem to struggle the most with acceptance. A lot of times, later on, they’ll graduate, and they’ll come back to me and say ‘Look at how far this kid has come.’ ”
She shares a helpful mindset for parents. “Tell yourself: Not yet. It doesn’t mean not ever. Your kid just isn’t there now.”
Beneath the Surface
What you see:
Standing on line in the supermarket, a woman is startled by a loud, exuberant shriek. She turns around and sees a teenage girl gesticulating wildly at a cheap toy on the endcap, then jumping up and down and clapping. What on earth? thinks the woman irritably. Even if her older sister had just gotten engaged, this is hardly the place for such displays of excitement. And the mother is just standing there and smiling at her daughter! Shaking her head, the woman turns back to her groceries.
What you don’t see:
This teenage girl was diagnosed with dyslexia when she was six, OCD when she was eight, then anxiety and ADHD a little later on. At 14, when she was still struggling, she received a diagnosis of autism.
High-functioning autism can be very challenging. A person with ASD can have the language and cognitive skills to be in a typical environment, but can lack the social, communication, and executive functioning skills to function well. Emotions can be felt more intensely, and are harder to regulate. This can explain why a teenage girl could have an outsized reaction to seeing her favorite toy in the supermarket.
Additionally, a person with ASD might also have a sensory processing disorder, anxiety, or other issues that make bright lights or loud noises almost impossible to manage.
Beneath the Surface
What you see:
An eight-year-old boy is in the dentist’s chair. The hygienist asks him to open his mouth, but he is refuses, repeatedly turning his head away and keeping his mouth tightly closed. The exasperated hygienist asks his mother to assist. He eventually agrees to open his mouth slightly, and even then keeps closing it. The hygienist is becoming impatient, and his mother is frustrated and angry with her son, the hygienist, and herself.
What you don’t see:
This boy didn’t yet have a diagnosis, though his parents had been trying to get to the bottom of his behavioral issues for a couple of years. He will eventually be diagnosed with ADHD, ODD (oppositional defiant disorder), and MDD (major depressive disorder).
ODD is more common in boys than girls, and is often found with other behavior and mood disorders, like ADHD and anxiety. Some symptoms might be more frequent temper tantrums, arguing a lot with adults, refusing to do what an adult asks, being easily annoyed with others, and often having an angry attitude.
Sometimes it’s difficult to recognize the difference between a strong-willed or emotional child and one with oppositional defiant disorder.
It’s normal to exhibit oppositional behavior at certain stages of a child’s development. Signs of ODD generally begin during preschool years. Sometimes ODD may develop later, but almost always before the early teen years. These behaviors cause significant impairment with family, social activities, school, and work.
Beneath the Surface
What you see:
It’s Shabbos afternoon, and a group of mothers get together with their little ones. After one little boy pushes a little girl one too many times, her mom turns to this boy’s mother, and says, point-blank, “You need to parent your child.”
“Sorry,” mutters his mortified mother.
What you don’t see:
This boy’s mother was in middle of having him evaluated. He was ultimately diagnosed with an extreme case of ADHD as well as anxiety. “The head of neurology saw my kid and said ‘Wow!’ ” the mom recalls.
ADHD (Attention deficit hyperactivity disorder) is often associated with nonstop movement and difficulty focusing, and while it may sometimes present like that, it’s more complex than that. The symptoms may present as hyperactivity, impulsivity, constant talking, and difficulty waiting. Other times they manifest as disorganization, inability to manage time, avoiding tasks that take sustained mental effort, being easily distracted, and making careless mistakes at work. Sometimes it’s a combination.
In addition to the long list of behavioral challenges that come with the condition, children with ADHD tend to be three to four years less mature than neurotypical children the same age, so a seventh grader with ADHD may act more like a third or fourth grader.
Beneath the Surface
What you see:
A grandmother takes her granddaughter out for a manicure, hoping for some quality bonding time. But instead of smiling and chitchatting while picking out colors she wants, the girl is asking nonstop questions like, “I don’t know, should I have come? Should I not have come? Should I have stayed home? Should I have done this?” Her grandmother is at a loss — this was supposed to be such a nice outing. Can’t they just enjoy themselves?
What you don’t see:
This girl has a diagnosis of Asperger’s, ADHD, and anxiety. While all these conditions make life challenging, right now it’s her anxiety that’s preventing her from enjoying herself.
Occasional anxiety is an expected part of life. A person might feel anxious when faced with a problem at work, before taking a test, or before making an important decision. But anxiety disorders involve more than temporary worry or fear. For a person with an anxiety disorder, the anxiety doesn’t go away and can get worse over time.
Anxiety may present as fear or worry, but can also make children irritable and angry. Anxiety symptoms can also include trouble sleeping, as well as physical symptoms like fatigue, headaches, or stomachaches. Some anxious children keep their worries to themselves, which means the symptoms can be missed.
Helpful Bystander
When you’re witnessing someone experience a difficult public parenting moment, it can be hard to know what to do. Some parents want validation while others just want to be left alone to deal with their child. Here are ways you can help.
React with empathy
“Understand that there are always things going on behind the scenes that you don’t know about. And if you think you know what’s going on — you don’t, by the way — but if you think you do, do your best to help out. Approach with empathy, from a perspective of ‘How do I support him and maybe give him a little chizuk?’ Start up a pareve conversation, and see if there’s an opportunity for some helpful advice from an ‘I’ve been there, I get it’ sort of place. Give a friendly smile and share what’s worked for you. Validate.”
—Dr. Benjamin Miller
“I don’t want to be embarrassed to take my kid out grocery shopping or whatever, because this is the way Hashem made her. She’s perfect the way she is, and I’ve accepted it, even though it’s hard at times. We need the community to accept it as well. Be kind, don’t stare.”
—Baila
Teach your kids to empathize
“Just because you’re empathetic doesn’t mean your child is empathetic.”
—Rachel
“I have one niece that has obvious special needs, and the other kids are always so nice to her, including her and inviting her, it’s a chesed. But they don’t treat my daughter like a chesed, they treat her like she’s annoying.”
—Hudy
“We need to educate our kids that there’s something called autism and Asperger’s, and kids with these conditions are going to behave unexpectedly, but they’re still great kids. They’re not neurotypical, but you can still be friends with them and you can have a relationship with them,”
—Baila
Offer to help
“My closest friends will help me and take her out. They give me a break. They’ll tell her ‘come with us, let’s go for a ride, let’s go get some ice cream,’ something like that.’ ”
—Baila
“One parent has been amazing and tried to create opportunities for her son to come over and hang out, but we’ve had to be okay with the fact that not everyone wants to hang out here all the time.”
—Rachel
Educate yourself
“The symptoms aren’t the result of a person being defiant or hostile or unable to understand a task or instructions, though it can certainly seem that way sometimes. Ask yourself ‘is that behavior defiance, or is that behavior a result of their disability?’ You can’t reprimand something that is not the child’s fault. You can’t punish a child for something that isn’t in his control.”
—Dassi Shtern
“You can say, ‘Well that kid just needs meds — just give him Ritalin and he’ll be fine.’ No. Meds solve 60 percent of the problem. That 60 percent for the teacher is huge. I do think that meds will help kids have more successful relationships with their teachers and oftentimes at home. I find without meds they don’t even have a fighting chance to learn new stuff. They don’t have the tools. Their brain isn’t working the way someone else’s brain is working to acquire or implement changes. But that’s only 60 percent of the way. The rest of it is behavior and learning tips and tricks. The 40 percent that’s left is meeting kids where they’re at — and teaching the community to be empathetic to people who are different than them.”
—Rachel
(Originally featured in Family First, Issue 787)
Oops! We could not locate your form.